VINEGAR OR ACETALDEHYDE – A COMMON AND POTENT NEUROTOXIN
Updated: Jun 30, 2022
A SECONDARY METABOLITE OF SUGAR CONSUMPTION
How to prevent the damaging effects of sugar consumption, smoking, alcohol consumption, and air pollution
Overcoming Addiction
Acetaldehyde is hardly a household word in America, yet it is one of the most common neurotoxins in the lives of tens of millions of people. It is a simple substance its chemical formula is CH3CHO yet acetaldehyde insidiously promotes damage to brain structure and function through numerous pathways.

Sources of Vinegar or Acetaldehyde
There are five main routes that bring acetaldehyde (abbreviated here as “AH”) into the human brain. These are sugar consumption, alcohol consumption, Candida “the yeast syndrome,” exhaust from cars and trucks, and cigarette smoking.
Ethanol (more commonly known as alcohol) is the chemical contained in beer, wine, liquor and liqueurs that gets people drunk. These beverages serve as carriers to get ethanol into the drinker’s brain, promoting some degree of intoxication.
Once in the body, alcohol is broken down into carbon dioxide and water. However, this process takes time and occurs in several steps. The first step occurs primarily in the liver, although other organs such as the brain and kidney can also perform this stage of alcohol detoxification to a slight extent. An enzyme called “alcohol dehydrogenase” converts alcohol into AH. Then another enzyme “aldehyde dehydrogenase” must break the AH down into acetate. Acetate can then serve as a fuel in cellular energy production. (Acetate is a form of acetic acid, the acid that makes vinegar sour.)
However, the conversion of AH to acetate does not always occur quickly or smoothly and therein lies the problem.
Research over the last several decades has shown that alcoholics tend to rapidly convert alcohol to AH, but then convert AH to acetate very slowly, thus giving AH a chance to work its mischief in the body.[1] And depending on a person’s genetics, nutritional status, and exposure to other chemicals such as formaldehyde, which also utilize aldehyde dehydrogenase for their detoxification, even non-alcoholics may have difficulty rapidly detoxifying AH.
The second major route of AH into the brain is through its production by a yeast called Candida albicans. Candida is known to occur in the intestinal tract of virtually all humans to some degree. When present only in small amounts, being kept in check by a healthy immune system and the so-called “friendly flora,” such as Acidophilus and Bifidus bacteria, Candida is relatively harmless. Yet due to the modern overuse of antibiotics, birth control pills, and cortisone/prednisone drug therapy, as well as excessive stress (which naturally produces excess cortisone in the body), sugar consumption and malnutrition, millions of Americans now suffer from an excessive growth of Candida in their intestines the so-called “yeast syndrome.”[2]
Candida thrives by fermenting sugars to produce energy.
Unfortunately for the humans who harbor large colonies of Candida in their gut, the waste by-product of this sugar fermentation by Candida is AH.[3] Biochemical research has shown that this AH may combine with red blood cells, proteins, enzymes, and other substances present in the gut or gut lining, and thus travel through the bloodstream to reach more distant parts of the body such as the brain.[3]
Research has also shown that AH can then detach from the red blood cells or proteins it traveled with through the bloodstream, thus enabling AH to damage cells far from the site of its intestinal production by Candida.[3]
For those suffering from the yeast syndrome, the ingestion of beer, wine, and liqueurs provides a double-barreled dose of AH. Not only is the alcohol in these beverages turned into AH, but the malt and grain in beer and the sugar in wine and liqueurs provide excellent fuel for Candida to produce the energy it needs to live.[2] More AH is the inevitable by-product of the yeast’s sugar fermentation.
When oil, gasoline, diesel fuel, and natural gas are burned, ending up in the air, AH is produced.[4] Thus, another major route of entry into the body for AH is through inhaling air laden with vehicle and factory exhaust. People who spend hours commuting in dense freeway traffic, professional drivers such as truck and taxi drivers in urban areas, and even those who live or work in heavily trafficked areas or near freeways or major streets are especially at risk for inhaling small but significant chronic levels of AH.
AH is also produced through the burning of tobacco.[7] Thus, heavy cigarette smokers are also at risk of inhaling AH through the inhaled smoke. And while the amounts of AH inhaled through auto exhaust and cigarette smoke may be small compared to that from alcohol, research shows that low-dose chronic AH exposure may still be sufficient to gradually damage proteins, enzymes and other cellular structures in the brain and other organs.[21]
How Vinegar or Acetaldehyde Damages the Brain There are many ways that acetaldehyde (AH) can gradually damage brain structure and function through chronic, low-dose AH exposure. The following are some of them.
Acetaldehyde alters red blood cell structure. It has been known since 1941 that AH easily combines with red blood cell membrane proteins to convert the red blood cells into a “time-release capsule” for AH, releasing the AH in the body far from the site where it attached to the red blood cell.[3]
As this happens, however, the membrane covering the red blood cell becomes stiffer.[21] Yet in order to travel through the capillaries, which are the smallest blood vessels and which feed the trillions of individual cells, the red blood cell must be able to fold or deform. The average red blood cell diameter is 7 microns; yet a typical capillary is only 2 microns in diameter. Red blood cells stiffened through chronic AH exposure will have difficulty deforming sufficiently to pass through capillaries. Consequently, red blood cell-carried oxygen to many cells is reduced.[3] (Our brains require 20% of all the oxygen we breathe!)
In addition, the work of K.K. Tsuboi and colleagues has shown that AH forms stable combinations with hemoglobin in red blood cells. This reduces the ability of red blood cells to accept, hold, and transport oxygen through the bloodstream, which is their primary function.[5]
Acetaldehyde decreases the ability of the protein tubulin to assemble into microtubules.[6] Microtubules are long, thin, tube-like structures that serve several functions in the brain cell. They help provide structural support to the nerve cell, somewhat like girders in a bridge or a building, keeping the nerve cell and the dendrites semi-rigid. Dendrites are the feathery-looking extensions from the main body of the nerve cell which connect nerve cells to each other, with some neurons connecting through dendrites to as many as 100,000 other neurons. Microtubules also serve to transport nutrients and biochemical raw materials manufactured in the cell body to the dendrites. When this raw material transport is compromised, the dendrites will gradually atrophy and die off.
Two classic examples of brain pathology involving degeneration of the dendrites in humans are chronic alcoholic brain damage and Alzheimer’s disease. Acetaldehyde induces a deficiency of vitamin B1. Thiamin, or Vitamin B1, is so critical to brain and nerve function it is often called the “nerve vitamin.” AH has a very strong tendency to combine with B1, as the work of Herbert Sprince, M.D. (discussed below) has shown.[7] Unfortunately, in detoxifying AH through combination with it, B1 is destroyed. Moderately severe B1 deficiency in humans leads to a group of symptoms called Wernicke-Korsakoff syndrome.[9]
This syndrome is characterized by mental confusion, poor memory, poor neuromuscular coordination, and visual disturbances. Its primary accepted cause is chronic alcoholism. B1 is also necessary for the production of ATP bioenergy in all body cells including the brain, and the brain must produce and use 20% of the body’s energy total, even while asleep. Vitamin B1 is also essential for production of acetylcholine. Acetylcholine is one of the brain’s major neurotransmitters, facilitating optimal memory, mental focus and concentration, and learning. Alzheimer’s disease represents a rather extreme case of memory loss and impaired concentration due to destruction of acetylcholine-using brain cells.
In a classic experiment reported in 1942, R.R. Williams and colleagues found that even mild B1 deficiency in humans continued over a long period of time (the experiment ran six months) produces symptoms including apathy, confusion, emotional instability, irritability, depression, feelings of impending doom, fatigue, insomnia, and headaches[8] all symptoms of less-than-optimal brain function.
Acetaldehyde induces deficiencies of Niacin and NAD
Niacin (Vitamin B3) is present in the human body primarily in its coenzyme form, NAD.[1]
NAD is involved in the majority of steps in which sugar and fat are burned for energy in all cells.[10]
NAD is normally the most plentiful vitamin coenzyme in the human brain.
NAD is important as a catalyst in the production of many key, brain neurotransmitters, such as serotonin.
Neurotransmitters are the biochemicals that allow nerve cells to communicate with each other.
NAD is also the coenzyme that activates alcohol dehydrogenase and aldehyde dehydrogenase, the enzymes that break down alcohol and AH.[11]
Zinc is also required along with NAD to activate these two enzymes.[12]
Since the need for NAD in all cells is great, yet the supply is limited, NAD is normally recycled continually during cellular energy production. Yet, when NAD helps detoxify AH, this recycling of NAD is blocked, and an altered form of NAD called “NADH” accumulates, impairing cellular biochemistry in many ways.[1][21]
Thus, chronic AH exposure may produce a mild, functional, niacin/NAD deficiency, even in a person consuming a so-called “balanced diet” which meets RDA levels of niacin intake.
Extreme niacin deficiency produces the classic nutritional disease Pellegra with dramatic symptoms, both physical and mental. Since niacin is needed in large amounts for optimal brain function, a mild niacin deficiency tends to produce mostly psychological symptoms. These symptoms may include feeling fearful, apprehensive, suspicious, and worrying excessively with a gloomy, downcast, angry and depressed outlook. Headaches, insomnia, depression, agitation, and inability to concentrate may also occur.[13]
This profile certainly applies to many chronic alcoholics and Candida patients, who obviously suffer from long-term, mild AH exposure.
Acetaldehyde reduces Acetyl Coenzyme A and impairs cellular energy production. Pantothenic Acid (Vitamin B5) is one of the most critical vitamins for normal brain function.
The active form of B5 is Coenzyme A. Coenzyme A in turn is combined with acetate in all cells to form Acetyl Coenzyme A. Acetyl Coenzyme A is perhaps the most pivotal single biochemical in all cellular biochemistry; both sugar and fat must be transformed into Acetyl Coenzyme A to power the Krebs’ cycle which produces 90% of all the energy used by every cell in the body, including brain cells.[11]
Unfortunately, for Acetyl Coenzyme A, however, AH has a strong affinity to combine with Acetyl Coenzyme A. The work of biochemist H.P. Ammon has shown that AH suppresses the activity of Acetyl Coenzyme A in a dose-dependent fashion. He has also demonstrated that the energy-producing activity of cells falls in parallel with the declining levels of Acetyl Coenzyme A as the concentration of AH increases.[1] The brain use. 20% of all body energy for normal function. Acetyl Coenzyme A is also necessary for the production of acetylcholine, the memory, learning and concentration neurotransmitter.[14]
Acetaldehyde induces a deficiency of Pyridoxal-5-Phosphate (P5P). P5P is the major coenzyme necessary to form virtually all major brain neurotransmitters.[10] It is involved in all transamination reactions, whereby cells may convert many different amino acids into each other to satisfy their ever-shifting amino acid needs.[10] P5P is necessary to convert essential fatty acids into their final use forms, as well as to turn linoleic acid into the key, nerve cell-regulating biochemical, Prostaglandin E1.[15] P5P helps regulate magnesium entry into cells,[16] and the level of excitability of nerve cells is strongly dependent upon their magnesium level. P5P is also necessary to convert vitamin B3, niacin/niacinamide, into the active coenzyme form, NAD.[17] Unfortunately for P5P (and we humans who are so dependent on it), AH is known to strongly combine with the protein portion of P5P enzymes in a way that displaces the P5P portion of the molecule. This subjects P5P to an increased rate of destruction and results in abnormally low blood and tissue levels of this coenzyme.[1][18]
Acetaldehyde unfavorably influences prostaglandin metabolism.
Delta-6-Desaturase is the enzyme that converts the common fatty acid linoleic acid into gamma linolenic acid, which is totally absent from any typical diet. Gamma linolenic acid in turn is the only raw material that can be converted into prostaglandin E1. Prostaglandin E1 is a key regulatory biochemical for both nerve cells and the immune system. It also serves to regulate the production of the pro-inflammatory prostaglandin E2. Prostaglandin E1 prevents excessive production of prostaglandin E2 from the dietary fatty acid, arachidonic acid, which is plentiful in meat, poultry and dairy products.
Researchers in prostaglandin biochemistry have discovered, however, that AH is a powerful deactivator of Delta-6-Desaturase.[15] AH thus tends to suppress gamma linolenic acid production, which in turn suppresses prostaglandin E1 production. Low prostaglandin E1 production “takes the brakes off” production of prostaglandin E2 and a related compound, TXB2, increasing their levels far above normal. The published research of David Horrobin, M.D.,[15] and psychiatrist Julian Lieb,19 has shown high levels of prostaglandin E2 and TXB2, coupled with low levels of prostaglandin E1, to be a major causal factor in some forms of depression.
Acetaldehyde promotes addiction to toxic substances
Perhaps one of the most surprising ways AH may alter normal brain function is due to its tendency to combine in the brain with two key neurotransmitters, dopamine and serotonin. When AH and dopamine combine, they form a condensation product called salsolinol. When AH combines with serotonin, another product called beta-carboline is formed. Salsolinol and beta-carboline are two of a group of inter-related and interconvertible compounds called tetrahydro-isoquinolines. The various tetrahydro-isoquinolines which both animal and human research have shown to occur at high levels in the brains, spinal fluids, and urine of chronic alcoholics are closely related in structure, function, and addictive power to opiates!
Successfully detoxifying alcoholics have been shown to excrete especially high levels of these opiate-like chemicals in their urine. Thus, these AH-generated, opiate-like biochemicals may at least partly explain why alcoholics are so addicted to alcohol, cigarette smokers to cigarettes, and Candida-sufferers to sugar, since all three of these conditions promote chronic excessive body AH levels. And, like opiates, these tetrahydroisoquinoline biochemicals would tend to promote lethargy, mental cloudiness and fogginess, depression, apathy, inability to concentrate, etc. These, of course, are symptoms common to both alcoholism and Candidiasis, the two conditions which would tend to generate the highest chronic AH levels in the body
The difficulties discussed above that are caused by chronic AH toxicity should indicate to the reader that AH has a significant ability to compromise brain function.
A partial summary of AH’s damaging effects on brain function includes the following:
Impaired memory
Decreased ability to concentrate (“brain fog”)
Depression
Slowed reflexes
Lethargy and apathy
Heightened irritability
Decreased mental energy
Increased anxiety and panic reactions
Decreased sensory acuity
Increased tendency to alcohol, sugar, and cigarette addiction
Decreased sex drive
Increased PMS and breast swelling/tenderness in women.
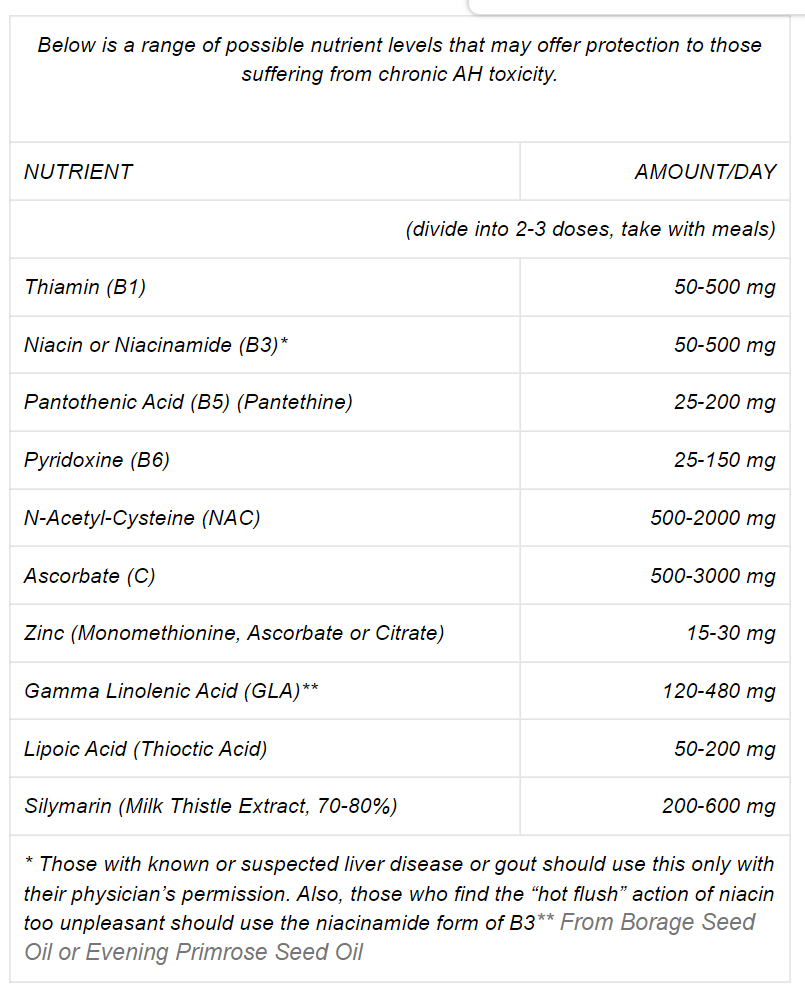
How Nutrition Can Help
Fortunately, applied nutrition science offers some protection against chronic AH toxicity, even when it is not possible to completely avoid the four main offenders that promote AH in our bodies alcohol, Candida, cigarettes, and heavy auto exhaust.
Herbert Sprince, M.D. and his colleagues published many articles in the 1970’s detailing the results of their experiments which used various nutrients to protect rats from AH poisoning.
Sprince fed a control group of rats an amount of AH sufficient to kill 90% of the control group in 72 hours. The experimental group of rats given the same amount of AH were also given various nutrients, either singly or in combination, that might detoxify the AH. After 72 hours, the death rate for rats given large oral doses of Vitamin C was only 27% (vs 90% in controls), 20% for rats given the sulfur amino acid L-cysteine, 10% for rats receiving Vitamin B1, and an amazing 0% for rats protected by N-acetyl cysteine or lipoic acid. A lower dose combination of C, B1 and either L-Cysteine or N-acetyl cysteine also gave near 0% death rates![7] But, the nutrient doses Sprince administered were rather gigantic compared to RDA levels of nutrients, being equivalent to multi-gram doses for humans.
Fortunately, however, most people are not subjected to such high levels of AH, so lower doses of these nutrients would doubtless provide significant AH-detoxifying power when used on a long-term basis.
John Cleary, M.D. has published papers summarizing many doctors’ and researchers’ successful use of niacin (Vitamin B3) and zinc in alcohol and AH detoxification.1 Since the enzymes that break down alcohol and AH are both B3[11] and zinc-activated,[12] this provides an obvious rationale for their protective use in chronic alcohol/AH toxicity situations. Finally, because chronic high tissue levels of AH impair the normal process of recycling the active form of B3 (NAD) for continual re-use,[1] it is obvious why normal dietary levels of B3 might be insufficient to provide optimal brain B3 levels in chronic AH toxicity situations.
References:
1. Cleary, J.P. The NAD Deficiency Diseases. J Orthomolecular Med, 1986, 1:164-74.
2. Galland, L.D. Nutrition and Candida Albicans, 1986 A Year in Nutritional Medicine, ed J. Bland. New Canaan:Keats Pub., 1986, 203-238.
3. Truss, C.O. Metabolic Abnormalities in Patients with Chronic Candidiasis: The Acetaldehyde Hypothesis. J Orthomolecular Psychiatry, 1984, 13:66-93.
4. Levine, S. and Kidd, P. Antioxidant Adaptation, pp. 70-71. San Francisco: Biocurrents Pub., 1986.
5. Tsuboi, K.K. et al. Acetaldehyde-Dependent Changes in Hemoglobin and Oxygen Affinity of Human Erythrocytes. Hemoglobin, 1981, 5:241-50.
6. Tuma, D.J. et al. The Interaction of Acetaldehyde with Tubulin, in: Ann NY Acad Sci, ed. E. Rubin, Vol. 492, 1987.
7. Sprince, H., et al. Protective Action of Ascorbic Acid and Sulfur Compounds against Acetaldehyde Toxicity: Implications in Alcoholism and Smoking. Agents and Actions, 1975, 5:164-73.
8. Williams, R.R., et al. Induced Thiamin (Vitamin B1) Deficiency in Man. Arch Int Med, 1942, 69:721-38.
9. Dreyfus, P.M. and Victor, M. Effects of Thiamine Deficiency on the Central Nervous System. Am J Clin Nutr, 1971, 9:414-25.
10. Kutsky, R.J. Handbook of Vitamins, Minerals, and Hormones, 2nd ed, p. 284. NYC: Van Nostrand Reinhold, 1981.
11. Lehninger, A.L. Principles of Biochemistry, p. 761. NYC: Worth Pub., 1982.
12. Das, I., et al. Effects of Zinc Deficiency on Ethanol Metabolism and Alcohol and Aldehyde Dehydrogenase Activities. J Lab Clin Med, 1984, 104:610-17.
13. Lesser, M. Nutrition and Vitamin Therapy, pp. 41-50. NYC: Bantam, 1981.
14. Pike, R.L. and Brown, M.L. Nutrition, An Integrated Approach, 3rd ed., pp 624. NYC: Macmillian Pub., 1984.
15. Horrobin, D.F. The Importance of Gamma-Linolenic Acid and Prostaglandin E1 in Human Nutrition and Medicine. J Holistic Med, 1981, 3:118-39.
16. Abraham, G.E., et al. Effect of Vitamin B6 on Plasma and Red Blood Cell Magnesium Levels in Premenopausal Woman. Ann Clin Lab Sci, 1981, 11:333-36.
17. Hoffer, A. Orthomolecular Medicine for Physicians, p. 34. New Canaan: Keats Pub, 1989.
18. Lumeng, L. The Role of Acetaldehyde in Mediating the Deleterious Effect of Ethanol on Pyridoxal-5-Phosphate Metabolism. J Clin Invest, 1978, 62:286-93.
19. Lieb, J. Elevated Levels of Prostaglandin E2 and Thromboxane B2 in Depression. Prost Leukotr Med, 1983, 10:361-67.
20. Blum, K. and Payne, J. Alcohol and the Addictive Brain, pp. 99- 216. NYC: The Free Press, 1991.
21. Sorrell, M.F. and Tuma, D.J. The Functional Implications of Acetaldehyde Binding to Cell Constituents; Ann NY Acad Sci, ed. E. Rubin, 1987, Vol. 492.
22. Cleary, J.P. Etiology and Biological Treatment of Alcohol Addiction. J Neurol Orthop Med Surg, 1985, 6:75-77.



