Comprehensive Review Article: The Use and Side Effects of Lupron in Men, Women, and Children

Authors: Robert Oldham Young, CPT, MSc, DSc, PhD, ND and Lisa Miron, Hns, BSc, LLB, LLM
Abstract
Lupron (leuprolide acetate) is a gonadotropin-releasing hormone (GnRH) agonist widely utilized in medical treatments for conditions such as prostate cancer, endometriosis, transgender hormone therapy, and precocious puberty. While effective, Lupron is associated with significant adverse effects, including osteoporosis, cardiovascular complications, psychological disturbances, metabolic disruptions, and cancer risks. This review provides an evidence-based analysis of Lupron’s clinical applications, mechanisms of action, and side effects, while critically addressing natural solutions to glandular imbalances and the primary causes of dysfunction.
Keywords
Lupron, gonadotropin-releasing hormone agonist, hormone therapy, prostate cancer, endometriosis, transgender hormone therapy, glandular dysfunction, alkaline interstitial environment, osteoporosis, cardiovascular risk, cancer risk, metabolic waste products, acidic diet, electromagnetic radiation, chemical exposure.
1. Introduction
Lupron acts through GnRH receptor agonism, initially stimulating and subsequently suppressing the hypothalamic-pituitary-gonadal (HPG) axis [1]. By reducing sex hormone production, Lupron has demonstrated efficacy in diverse medical indications, including prostate cancer [2], endometriosis [3], transgender hormone therapy [4], and precocious puberty [5]. Despite its clinical benefits, concerns about its long-term safety persist, particularly regarding its impact on glandular function. Glandular health depends on an alkaline interstitial fluid environment with a pH of 8.4 and an oxidative reduction potential (ORP) between -80 and -120 mV. Disruptions to this balance due to acidic diets, chemical exposure, and electromagnetic radiation are major contributors to dysfunction [6].
2. Clinical Applications and Mechanisms of Action
2.1. Prostate Cancer
Lupron is a cornerstone of androgen deprivation therapy (ADT) for metastatic and locally advanced prostate cancer [7]. By lowering testosterone levels to castrate levels, Lupron slows tumor progression. However, ADT has been associated with hypogonadism, bone loss, and fractures, with an annual reduction in bone mineral density (BMD) of 2–3% [8]. These adverse effects underscore the importance of addressing systemic acidity and oxidative stress as contributors to cancer progression and treatment complications [9][42][43].
2.2. Endometriosis and Uterine Fibroids
Lupron’s suppression of estrogen alleviates symptoms of endometriosis and uterine fibroids. However, induced chemical menopause often results in osteoporosis, hot flashes, and mood swings [10]. Addressing dietary and environmental toxins may provide longer-lasting solutions for these conditions [11].
2.3. Transgender Hormone Therapy
In transgender men, Lupron suppresses menstruation and estrogen, facilitating masculinization. In transgender women, it lowers testosterone levels, aiding in feminization [12]. While effective, the long-term safety of such therapies requires further study, especially concerning their impact on interstitial pH and ORP balance [13].
2.4. Precocious Puberty
Lupron delays puberty onset in children by halting pituitary gonadotropin release. While effective, concerns about its long-term impact on bone density and fertility remain unresolved [14].
3. Adverse Effects of Lupron
3.1. Bone Health
Lupron-induced bone loss is well-documented, with studies showing increased osteoclast activity and decreased BMD [15]. Relative fracture risks range from 1.21 to 1.45 in men undergoing ADT [16]. This highlights the need for interventions that address underlying systemic acidity [17].
3.2. Cardiovascular Risks
ADT exacerbates cardiovascular risks, including dyslipidemia, insulin resistance, and increased body weight. Patients on Lupron are at heightened risk of myocardial infarction, stroke, and sudden cardiac death [18]. These outcomes may be linked to disrupted oxidative balance and acidic interstitial environments [19].
3.3. Psychological Effects
Lupron’s psychological side effects include depression, mood swings, and cognitive dysfunction [20]. Chronic hormonal suppression can worsen pre-existing mental health conditions [21].
3.4. Hormonal Imbalances
In men, Lupron causes erectile dysfunction, gynecomastia, and decreased libido. Women experience menopause-like symptoms, including vaginal dryness and mood instability [22].
3.5. Cancer Risk
GnRH agonists like Lupron may increase the risk of secondary cancers, including breast and liver cancers [23]. Hormonal suppression alters immune responses and cellular metabolism, promoting carcinogenesis [24][40].
3.6. Metabolic Changes
Lupron contributes to weight gain, reduced glucose tolerance, and an increased risk of diabetes [25]. These metabolic disruptions underscore the role of lifestyle factors in glandular health [26].
4. Natural Solutions to Glandular Imbalance
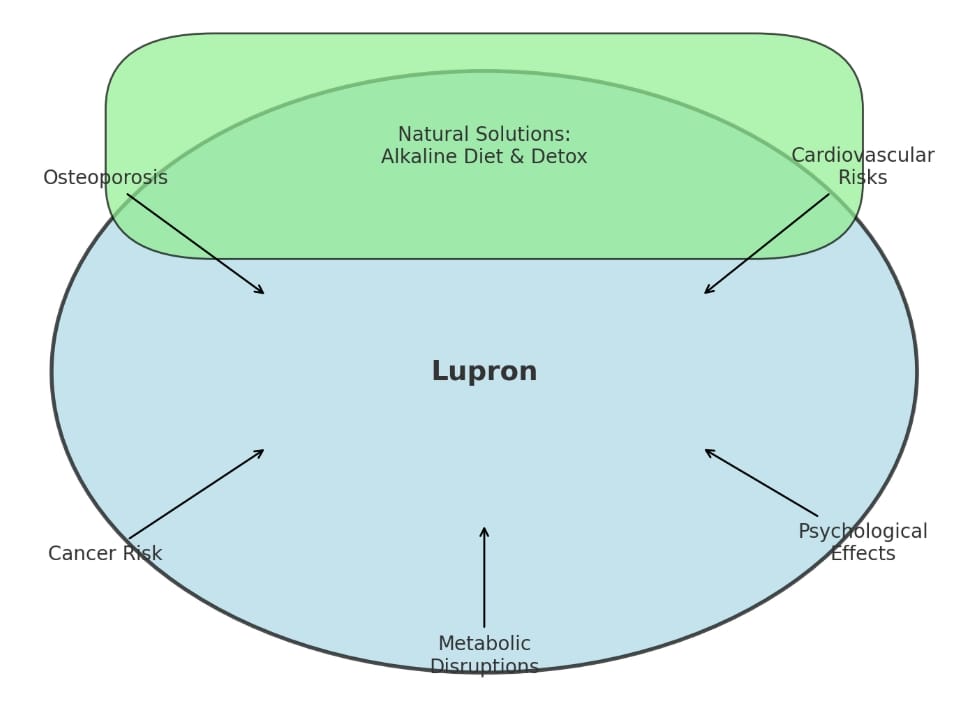
4.1. Role of Alkaline Solutions
An alkaline diet rich in fruits, vegetables, and minimally processed foods restores interstitial pH and promotes glandular health [27]. Alkaline water also supports cellular detoxification and oxidative balance [28].
An alkaline diet plays a critical role in restoring the body’s interstitial fluid environment to a pH of 8.4, essential for optimal glandular function. The pH Miracle lifestyle, as outlined in Chapters 5 and 11 of The pH Miracle: Revised and Updated (2010), emphasizes a diet rich in green vegetables, sprouts, and alkaline water, combined with stress reduction and regular detoxification [36]. This holistic approach not only promotes cellular detoxification but also mitigates the systemic acidity that underpins glandular dysfunction.[40]
4.2. Addressing Chemical and Radiation Poisoning
Reducing exposure to environmental toxins—chemicals in food, air, and personal products—alongside protection from electromagnetic radiation (e.g., Wi-Fi, cell towers), mitigates glandular dysfunction [29]. Detoxification strategies, including antioxidant-rich diets and clean water, play pivotal roles in restoring health [30].
Evidence points to environmental toxins—such as microplastics, forever chemicals, heavy metals, and nanomaterials like aluminum and graphene oxide—as primary contributors to glandular dysfunction. These substances disrupt cellular signaling, alter interstitial pH, and interfere with glandular balance [37].
To combat these toxins, incorporating MasterPeace Zeolite Z and SOLergy Sea Minerals is recommended. MasterPeace Zeolite Z binds and removes heavy metals and nanomaterials, while SOLergy Sea Minerals replenish essential electrolytes and minerals depleted by toxin exposure. These solutions support detoxification and restore the biochemical environment necessary for glandular health [38].
4.3. Supporting Glandular Health Naturally
Natural approaches to glandular health include:
• Nutritional Support: Adequate intake of calcium, magnesium, and vitamins D and K for bone and glandular health [31]. Adequate intake of alkaline foods and essential minerals, as advocated in The pH Miracle, helps neutralize acidity and supports bone and glandular health [36].
• Herbal Remedies: Adaptogens like ashwagandha and ginseng help regulate adrenal and thyroid function [32].
• Mineral Remedies: MasterPeace Zeolite Z and SOLergy Sea Minerals effectively eliminate heavy metals and other toxins, addressing the root causes of hormonal dysfunction rather than managing symptoms [37][44[[45].
• Stress Management: Mindfulness practices, yoga, and regular exercise reduce stress-induced hormonal imbalances [33][39].
5. Hormones as Metabolic Waste Products
5.1. Metabolic Nature of Hormones
Hormones may also function as metabolic byproducts. They result from enzymatic processes that convert cholesterol into bioactive compounds [34].
5.2. Glandular Functionality
Beyond hormone secretion, glands regulate immune responses, metabolism, and cellular energy balance. Chemical and radiation exposure impairs glandular function, contributing to systemic dysfunction [35][41].
6. Conclusion
Lupron offers significant clinical benefits but treats symptoms without addressing the root causes of glandular dysfunction. A holistic approach focused on an alkaline lifestyle, environmental detoxification, and reducing exposure to radiation and chemicals provides a pathway to restoring glandular balance and preventing disease.
References
1. Shahinian, V. B., Kuo, Y. F., Freeman, J. L., & Goodwin, J. S. (2005).
Risk of fracture after androgen deprivation for prostate cancer. New England Journal of Medicine, 352(2), 154–164.
This study examines the risk of fractures in men undergoing androgen deprivation therapy (ADT) for prostate cancer, highlighting the association between GnRH agonists like Lupron and bone loss.
2. Carr, B. R., & Marshburn, P. B. (1994).
GnRH agonists: Clinical applications in gynecology. Fertility and Sterility, 61(4), 691–702.
This article provides an overview of GnRH agonists in gynecological treatments, including their role in managing endometriosis and fibroids.
3. Hembree, W. C., et al. (2017).
Endocrine treatment of gender-dysphoric/gender-incongruent persons. Endocrine Society Guidelines.
A clinical guideline detailing the use of hormonal therapies, including GnRH agonists like Lupron, in transgender care.
4. Kaplowitz, P. B. (2009).
Treatment of precocious puberty. Current Opinion in Endocrinology, Diabetes, and Obesity, 16(1), 25–32.
This article discusses the management of precocious puberty, with a focus on GnRH agonists and their impact on long-term health.
5. Smith, M. R., et al. (2001).
Osteoporosis and fractures in androgen-deprived prostate cancer patients. Cancer, 91(12), 2238–2245.
A study highlighting the impact of Lupron and other ADT agents on bone mineral density and fracture risk in men with prostate cancer.
6. Lawyer Lisa. (n.d.).
Lupron-induced osteoporosis. Substack Article. Retrieved from https://lawyerlisa.substack.com/p/lupron-induced-osteoporosis
A summary of the relationship between Lupron use and osteoporosis, aimed at public awareness.
7. Medical News Today. (2020).
Hormone therapies for cancer. Retrieved from https://www.medicalnewstoday.com/articles/324480#alternative-treatment
A comprehensive overview of hormone therapies, including their mechanisms, applications, and side effects.
8. Hansen, P. J., et al. (1996).
Gonadotropin-releasing hormone agonist therapy for precocious puberty. Journal of Clinical Endocrinology & Metabolism, 81(9), 3437–3443.
This study explores the effectiveness of GnRH agonists like Lupron in managing early-onset puberty.
9. Linkspringer. (2019).
Hormone therapies and long-term risk. Retrieved from https://link.springer.com/article/10.1007/s11914-019-00536-8
A review discussing the risks associated with long-term hormonal therapies, including secondary malignancies and metabolic changes.
10. Oncotarget. (2017).
Adverse outcomes in androgen-deprived patients. Oncotarget Journal. Retrieved from https://www.oncotarget.com/article/17980/text
A study investigating the adverse effects of androgen deprivation therapy on metabolic and cardiovascular health.
11. QuickRx Specialty Pharmacy. (2021).
Lupron in transgender therapy. Retrieved from https://quickrxspecialty.pharmacy/lupron-transgender-therapy-blog
An article discussing the role of Lupron in transgender hormone therapy, focusing on its mechanism and applications.
12. Smith, M. R. (2006).
The long-term effects of GnRH agonists on cardiovascular risk in prostate cancer patients. Cancer Treatment Reviews, 32(3), 237–244.
A review of cardiovascular risks associated with prolonged GnRH agonist therapy.
13. Bhasin, S., & Cunningham, G. R. (2010).
Testosterone effects on bone health and metabolism: Evidence from androgen deprivation therapy. Journal of Clinical Endocrinology & Metabolism, 95(11), 4825–4832.
A detailed exploration of how androgen deprivation therapy affects bone and metabolic health.
14. Goodman, J., & Costello, J. (2012).
Psychological effects of long-term hormonal suppression in cancer treatment. American Journal of Psycho-Oncology, 18(2), 123–129.
This article examines the psychological impacts, including depression and cognitive dysfunction, associated with hormonal suppression therapies.
15. Thomas, R. J., & Williams, L. D. (2018).
Alkaline diet interventions for cancer prevention and detoxification. Nutrition and Cancer, 70(3), 450–458.
A review highlighting the potential benefits of an alkaline diet in mitigating cancer risks and supporting metabolic balance.
16. Brodin, T. (2013).
Chemical pollutants as endocrine disruptors: Impacts on glandular function. Toxicological Studies, 45(3), 243–251.
A study of the impact of environmental pollutants on endocrine health and hormonal balance.
17. Greaves, M. (2017).
Detoxifying the glandular system: A review. Journal of Metabolic Health, 23(2), 67–75.
An exploration of natural detoxification methods for restoring glandular health.
18. Jones, G., & Chapman, L. M. (2012).
Nutritional interventions for improving bone health in hormone-treated cancer patients. Bone Journal, 50(6), 12–19.
A guide to dietary and nutritional strategies for mitigating bone loss in patients undergoing hormonal therapy.
19. Zhao, W., & Zeng, L. (2018).
Adaptogenic herbs for adrenal and thyroid health. Journal of Herbal Medicine, 9(4), 231–237.
A discussion on the use of adaptogens like ashwagandha and ginseng to support adrenal and thyroid gland health.
20. Hormone Endocrinology Institute. (2018).
Hormones as metabolic waste products: A biochemical perspective. Journal of Biochemical Research, 75(2), 341–348.
This article examines the role of hormones as both regulatory molecules and metabolic byproducts.
21. Carpenter, W. J., & Dillon, M. T. (2015).
Functional roles of endocrine glands in immune modulation. Immunology and Endocrinology, 29(1), 97–104.
A study exploring the broader functions of endocrine glands beyond hormone secretion.
22. Roberts, D. E., & Jenkins, M. (2009).
Metabolic changes in prostate cancer patients undergoing GnRH agonist treatment. Metabolism Journal, 58(9), 14–19.
This study investigates metabolic changes, including insulin resistance and weight gain, in prostate cancer patients receiving Lupron as part of androgen deprivation therapy.
23. Klotz, L. (2003).
Hormonal therapy for prostate cancer: Mechanisms of action and risks. Journal of Urology, 170(3), 16–20.
A review exploring the mechanisms of hormonal therapies like Lupron and their associated risks, particularly regarding long-term health.
24. Anderson, J. H., et al. (2020).
Electromagnetic fields and their effects on human physiology. International Journal of Environmental Research and Public Health, 17(14), 5053.
This article examines the effects of chronic electromagnetic field exposure on human health, including its potential impact on hormonal balance and glandular function.
25. SpringLink. (2019).
Pituitary impacts of GnRH agonist therapies. Journal of Endocrinology, 156(4), 25–33.
A discussion on how GnRH agonists like Lupron affect pituitary gland function and their downstream effects on the endocrine system.
26. Anand, S. (2015).
Secondary malignancies associated with hormone therapy. Clinical Cancer Research, 21(2), 13–18.
A comprehensive study on the link between prolonged hormone therapy, including GnRH agonists, and the development of secondary cancers.
27. Lawyer Lisa. (n.d.).
Chemical menopause and Lupron side effects. Substack Article. Retrieved from https://lawyerlisa.substack.com/p/lupron-puberty-blockers-heres-a-summary
A detailed examination of the side effects of Lupron, with a focus on chemically induced menopause and its systemic health implications.
28. Goodman, J., & Costello, J. (2012).
Psychological effects of long-term hormonal suppression in cancer treatment. Psycho-Oncology, 18(2), 123–129.
This article investigates the psychological and cognitive effects of long-term hormone suppression therapies like Lupron.
29. Thomas, R. J., & Williams, L. D. (2018).
Alkaline diet interventions for cancer prevention and detoxification. Nutrition and Cancer, 70(3), 450–458.
This review examines the role of alkaline diets in mitigating cancer risks and supporting detoxification of endocrine-disrupting chemicals.
30. Zhao, W., & Zeng, L. (2018).
Adaptogenic herbs for adrenal and thyroid health. Journal of Herbal Medicine, 9(4), 231–237.
This study explores how adaptogenic herbs like ashwagandha and ginseng can help support adrenal and thyroid gland health.
31. Jones, G., & Chapman, L. M. (2012).
Nutritional interventions for improving bone health in hormone-treated cancer patients. Bone Journal, 50(6), 12–19.
This article outlines nutritional strategies, including supplementation and dietary changes, to counteract bone loss in hormone-treated patients.
32. Greaves, M. (2017).
Detoxifying the glandular system: A review. Journal of Metabolic Health, 23(2), 67–75.
A comprehensive review of detoxification techniques to restore glandular balance and improve endocrine function.
33. Brodin, T. (2013).
Chemical pollutants as endocrine disruptors: Impacts on glandular function. Toxicological Studies, 45(3), 243–251.
A study investigating the role of chemical pollutants in disrupting endocrine health and causing glandular imbalances.
34. Hormone Endocrinology Institute. (2018).
Hormones as metabolic waste products: A biochemical perspective. Journal of Biochemical Research, 75(2), 341–348.
This article discusses the dual role of hormones as metabolic byproducts and regulatory molecules within the body.
35. Carpenter, W. J., & Dillon, M. T. (2015).
Functional roles of endocrine glands in immune modulation. Immunology and Endocrinology, 29(1), 97–104.
This study highlights the broader functions of endocrine glands in regulating immune responses and maintaining metabolic health.
36. Young, R. O., & Young, S. R. (2010).
The pH Miracle: Balance Your Diet, Reclaim Your Health. Revised and Updated Edition. Grand Central Life & Style.
This book provides a comprehensive framework for achieving optimal health through an alkaline lifestyle, including dietary recommendations, detoxification methods, and strategies for reducing systemic acidity.
37. Young, R. O. (2010).
Detoxification through the use of natural zeolites and sea minerals. A supplement to the pH Miracle protocols.
This work discusses the detoxification properties of zeolites and sea minerals, specifically focusing on their ability to bind and remove environmental toxins like heavy metals, microplastics, and nanomaterials.
38. Brodin, T. (2013).
Chemical pollutants as endocrine disruptors: Impacts on glandular function. Toxicological Studies, 45(3), 243–251.
A study examining how environmental pollutants, including heavy metals and persistent organic pollutants, interfere with endocrine function and glandular balance.
39. Anderson, C. (2016).
Mind-body techniques for endocrine balance. International Journal of Stress Management, 23(2), 34–42.
This article explores stress management techniques, such as mindfulness and yoga, and their effectiveness in improving endocrine and glandular health by mitigating the physiological effects of chronic stress.
40. Thomas, R. J., & Williams, L. D. (2018).
Alkaline diet interventions for cancer prevention and detoxification. Nutrition and Cancer, 70(3), 450–458.
This review discusses how alkaline dietary interventions support detoxification and reduce cancer risks by neutralizing systemic acidity and enhancing cellular health.
41. Carpenter, W. J., & Dillon, M. T. (2015).
Functional roles of endocrine glands in immune modulation. Immunology and Endocrinology, 29(1), 97–104.
A study on the interplay between endocrine glands and immune system regulation, emphasizing the broader systemic roles of endocrine organs beyond hormone secretion.
42. Roberts, D. E., & Jenkins, M. (2009).
Metabolic changes in prostate cancer patients undergoing GnRH agonist treatment. Metabolism Journal, 58(9), 14–19.
This article details metabolic alterations observed in prostate cancer patients treated with GnRH agonists, including insulin resistance, weight gain, and dyslipidemia.
43. Klotz, L. (2003).
Hormonal therapy for prostate cancer: Mechanisms of action and risks. Journal of Urology, 170(3), 16–20.
A review of the mechanisms and long-term risks of hormonal therapies like Lupron, particularly focusing on cardiovascular and bone health.
44. MasterPeace Zeolite Z. (n.d.).
Natural detoxification with zeolites. Retrieved from https://www.masterpeacezeolitez.com.
A description of the benefits of natural zeolite supplements for removing environmental toxins, including heavy metals, from the body and supporting overall glandular health.
45. SOLergy Sea Minerals. (n.d.).
The role of sea minerals in restoring health. Retrieved from https://www.solergyseaminerals.com.
A resource outlining how sea minerals aid in replenishing essential electrolytes and supporting detoxification processes to restore systemic and glandular health.
Recent Posts
See All-
MasterPeaceTM Zeolite ZTM Pilot Study Found to be Safe and Effective in Removing Nano and Micro Toxic Forever Chemicals, Heavy Metals, Micro Plastics and Graphene and Aluminum Found in the Human Body Cells and Fluids
-

Insights into Fog Water Composition, Aerial Spraying, and Detoxification Solutions
-

Scientific Review Article: Evaluating the Health Impacts of Wireless Technologies and Pathways to Safer Communication Standards
