Examining the Relationship Between Diet-Induced Acidosis and Cancer
Updated: Jun 30, 2022
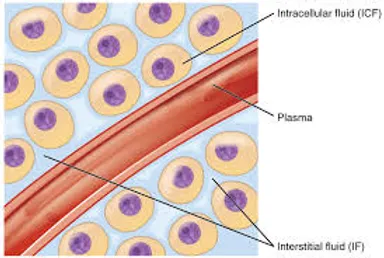
“What YOU Eat and What YOU Drink Does Effect the pH of the Blood and then the Interstitial Fluids of the Interstitium leading to health and vitality or sickness and disease.”
Dr. Robert O Young
“The single most important factor in human health is determined by what you eat!” Dr. Robert O Young
Abstract
Increased cancer risk is associated with select dietary factors. Dietary lifestyles can alter systemic acid-base balance over time. Acidogenic diets, which are typically high in animal protein and salt and low in fruits and vegetables, can lead to a sub-clinical or low-grade state of metabolic acidosis. The relationship between diet and cancer risk prompts questions about the role of acidosis in the initiation and progression of cancer. Cancer is triggered by genetic and epigenetic perturbations in the normal cell, but it has become clear that microenvironmental and systemic factors exert modifying effects on cancer cell development. While there are no studies showing a direct link between diet-induced acidosis and cancer, acid-base disequilibrium has been shown to modulate molecular activity including adrenal glucocorticoid, insulin growth factor (IGF-1), and adipocyte cytokine signaling, dysregulated cellular metabolism, and osteoclast activation, which may serve as intermediary or downstream effectors of carcinogenesis or tumor promotion. In short, diet-induced acidosis may influence molecular activities at the cellular level that promote carcinogenesis or tumor progression. This review defines the relationship between dietary lifestyle and acid-base balance and discusses the potential consequences of diet-induced acidosis and cancer occurrence or progression.
Diet, cancer, and ‘acidity’
The relationship between diet and cancer is well known [1-3]. Dietary intake exists as the largest external or environmental epigenetic factor capable of driving the development or maintenance of cancer. The American Institute for Cancer Research (AICR) comprehensive global report has compiled numerous studies demonstrating associations between dietary habits and cancer risk [4]. The findings recommend increased or regular consumption of vegetables, fruits, whole grains, and legumes, while discouraging excess consumption of sugary and energy-dense foods and drinks, red and processed meats, and salty processed foods (http://www.aicr.org).
Acidity is a well known factor associated with cancer. Lower pH levels in the extracellular space promote the invasive and metastatic potential of cancer cells [5-14]. Extracellular acidity is mostly generated by tumor cells due to upregulated proton [H+ and lactic acid production [15].
This phenomenon is distinct from ‘acidity’ caused by a net-acid diet. A net-acid diet or acidogenic diet is determined by the balance between acid and base-forming dietary constituents. Most fruits and vegetables are net-base producing foods since the metabolized products are organic anion precursors such as citrate, succinate, and conjugate bases of carboxylic acids [16-18]. The final metabolite of these precursors is bicarbonate anion. Sulfur containing amino acids, methionine and cysteine, typically found in meats, eggs and dairy products, are oxidized into sulfuric acid which is ultimately net-acid producing [16]. Cationic amino acids such as lysine and arginine can be acid producing if their anionic counterpart is chloride, sulfate, or phosphate. However, if the anionic component is a metabolizable organic acid (glutamate or aspartate), there is almost no impact on systemic acidity [17,18]. Other dietary factors are known to influence acid-base status as well. Sodium chloride is reported to be an independent and causal factor for inducing metabolic acidosis in a dose-dependent manner [19,20]. Conversely, potassium salts, and to a lesser degree magnesium, serve as a countervailing effect on net acid excretion and help to promote alkaline balance [21,22].

Acidogenic dietary intake such as high protein consumption can have an immediate effect on increasing net acid production while low protein lacto-vegetarian consumption can result in significantly reduced net acid excretion [23,24]. Short-term dietetic acid loading may cause temporary acid-base disequilibrium, but is quickly compensated and has no measureable clinical effect. A persistent acidogenic diet, however, raises the likelihood of an increased [H+ surplus and chronically lower levels of serum bicarbonate if compensatory processes become less efficient and are unresolved by dietary adjustments. Potential long-term effects of acidogenic diets are further compounded by the reduction of renal function typically from ageing [16,25-28].

Blood pH from prolonged or chronic acidogenic diets is reported to be near the lower physiological range (7.36-7.38) rather than the higher end (7.42-7.44). Specifically, persistent acidogenic diets have the potential to cause small decreases in blood pH and plasma bicarbonate, but not beyond the normal physiological range. This condition is described as ‘diet-induced’, ‘low-grade’, or ‘chronic metabolic acidosis’ [28-30] or sometimes ‘latent acidosis’ [31].
Diet-induced acidosis is distinct from clinical metabolic acidosis in that clinical metabolic acidosis occurs when factors other than just acidogenic diet contribute a system’s inability to compensate for blood [H+ perturbations, typically resulting in blood pH below 7.35 [32]. The patho-physiological effects of clinical metabolic acidosis are well known [33], while the true pathophysiological impact of long-term, diet-induced acidosis is not well understood. For example, it is unknown if [H+ accumulation from chronic diet-induced acidosis can be stored at the cellular level if it does not play a role in lowering blood pH or is compensated by competent renal or respiratory function. Studies of the impact of clinical metabolic acidosis on biological systems may still be informative towards understanding the effects of diet-induced acidosis because they examine how acid-base disequilibrium causes physiological stress and influences molecular pathways active in disease processes [34].
It is generally understood that the cancer condition evolves from genetic and epigenetic changes in the normal cell. Both microenvironmental and systemic factors exert selective pressures that aid in the initiation or aggravation of tumors.
Acid-base disequilibrium is considered a type of systemic stress. With the understanding that long-term acidogenic diets potentially exert chronic physiological stress, the question proposed here is:
Can diet-induced acidosis increase cancer risk or promote existing tumors?

References on Diet Induced Acidosis and Causing Cancer
1. Society AC, editor. American Cancer Society. Atlanta; 2004. Cancer Facts and Figures. http://www.cancer.org/acs/groups/content/@epidemiologysurveilance/documents/document/acspc-028323.pdf. [Google Scholar]
2, Calle EE, Kaaks R. Overweight, obesity and cancer: epidemiological evidence and proposed mechanisms. Nat Rev Cancer. 2004;4(8):579–591. [PubMed] [Google Scholar]
3. Hursting SD, Berger NA. Energy balance, host-related factors, and cancer progression. J Clin Oncol. 2010;28(26):4058–4065. doi: 10.1200/JCO.2010.27.9935. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
4. Research WCRFAIfC. Food, Nutrition, and Physical Activity, and the Prevention of Cancer: A Global Perspective. In. Washington DC: AICR; 2007. [Google Scholar]
5. Kato Y, Lambert CA, Colige AC, Mineur P, Noel A, Frankenne F, Foidart JM, Baba M, Hata R, Miyazaki K. et al.
6. Acidic extracellular pH induces matrix metalloproteinase-9 expression in mouse metastatic melanoma cells through the phospholipase D-mitogen-activated protein kinase signaling. J Biol Chem. 2005;280(12):10938–10944. doi: 10.1074/jbc.M411313200. [PubMed] [CrossRef] [Google Scholar]
7. Kato Y, Ozawa S, Tsukuda M, Kubota E, Miyazaki K, St-Pierre Y, Hata R. Acidic extracellular pH increases calcium influx-triggered phospholipase D activity along with acidic sphingomyelinase activation to induce matrix metalloproteinase-9 expression in mouse metastatic melanoma. FEBS J. 2007;274(12):3171–3183. doi: 10.1111/j.1742-4658.2007.05848.x. [PubMed] [CrossRef] [Google Scholar]
8. Martinez-Zaguilan R, Seftor EA, Seftor RE, Chu YW, Gillies RJ, Hendrix MJ. Acidic pH enhances the invasive behavior of human melanoma cells. Clin Exp Metastasis. 1996;14(2):176–186. doi: 10.1007/BF00121214. [PubMed] [CrossRef] [Google Scholar]
9. Moellering RE, Black KC, Krishnamurty C, Baggett BK, Stafford P, Rain M, Gatenby RA, Gillies RJ. Acid treatment of melanoma cells selects for invasive phenotypes. Clin Exp Metastasis. 2008;25(4):411–425. doi: 10.1007/s10585-008-9145-7. [PubMed] [CrossRef] [Google Scholar]
10. Rofstad EK, Mathiesen B, Kindem K, Galappathi K. Acidic extracellular pH promotes experimental metastasis of human melanoma cells in athymic nude mice. Cancer Res. 2006;66(13):6699–6707. doi: 10.1158/0008-5472.CAN-06-0983. [PubMed] [CrossRef] [Google Scholar]
11. Rozhin J, Sameni M, Ziegler G, Sloane BF. Pericellular pH affects distribution and secretion of cathepsin B in malignant cells. Cancer Res. 1994;54(24):6517–6525. [PubMed] [Google Scholar]
12. Shi Q, Le X, Wang B, Abbruzzese JL, Xiong Q, He Y, Xie K. Regulation of vascular endothelial growth factor expression by acidosis in human cancer cells. Oncogene. 2001;20(28):3751–3756. doi: 10.1038/sj.onc.1204500. [PubMed] [CrossRef] [Google Scholar]
13. Welbourne TC, Francoeur D. Influence of aldosterone on renal ammonia production. Am J Physiol. 1977;233(1):E56–E60. [PubMed] [Google Scholar]
14. Xu L, Fidler IJ. Acidic pH-induced elevation in interleukin 8 expression by human ovarian carcinoma cells. Cancer Res. 2000;60(16):4610–4616. [PubMed] [Google Scholar]
15. Xu L, Fukumura D, Jain RK. Acidic extracellular pH induces vascular endothelial growth factor (VEGF) in human glioblastoma cells via ERK1/2 MAPK signaling pathway: mechanism of low pH-induced VEGF. J Biol Chem. 2002;277(13):11368–11374. doi: 10.1074/jbc.M108347200. [PubMed] [CrossRef] [Google Scholar]
16. Schornack PA, Gillies RJ. Contributions of cell metabolism and H + diffusion to the acidic pH of tumors. Neoplasia. 2003;5(2):135–145. [PMC free article] [PubMed] [Google Scholar]
17. Cordain L, Eaton SB, Sebastian A, Mann N, Lindeberg S, Watkins BA, O’Keefe JH, Brand-Miller J. Origins and evolution of the Western diet: health implications for the 21st century. Am J Clin Nutr. 2005;81(2):341–354. [PubMed] [Google Scholar]
18. Halperin ML. Metabolism and acid-base physiology. Artif Organs. 1982;6(4):357–362. doi: 10.1111/j.1525-1594.1982.tb04126.x. [PubMed] [CrossRef] [Google Scholar]
19. Kleinman J, Lemann J. In: Clinical disorders of fluid and electrolyte metabolism. 4. Maxwell M, Kleeman C, Narins R, editor. New York: McGraw Hill; 1987. Acid Production; pp. 159–173. [Google Scholar]
20. Frassetto LA, Morris RC, Sebastian A. Dietary sodium chloride intake independently predicts the degree of hyperchloremic metabolic acidosis in healthy humans consuming a net acid-producing diet. Am J Physiol Renal Physiol. 2007;293(2):F521–F525. doi: 10.1152/ajprenal.00048.2007. [PubMed] [CrossRef] [Google Scholar]
21. Frings-Meuthen P, Baecker N, Heer M. Low-grade metabolic acidosis may be the cause of sodium chloride-induced exaggerated bone resorption. J Bone Miner Res. 2008;23(4):517–524. [PubMed] [Google Scholar]
22. Frassetto LA, Todd KM, Morris RC, Sebastian A. Estimation of net endogenous noncarbonic acid production in humans from diet potassium and protein contents. Am J Clin Nutr. 1998;68(3):576–583. [PubMed] [Google Scholar]
23. Remer T, Manz F. Paleolithic diet, sweet potato eaters, and potential renal acid load. Am J Clin Nutr. 2003;78(4):802–803. author reply 803-804. [PubMed] [Google Scholar]
24. Remer T, Manz F. Estimation of the renal net acid excretion by adults consuming diets containing variable amounts of protein. Am J Clin Nutr. 1994;59(6):1356–1361. [PubMed] [Google Scholar]
25. Remer T, Manz F. Dietary protein as a modulator of the renal net acid excretion capacity: Evidence that an increased protein intake improves the capability of the kidney to excrete ammonium. J Nutr Biochem. 1995;6:431–437. doi: 10.1016/0955-2863(95)00064-7. [CrossRef] [Google Scholar]
26. Frassetto L, Morris RC. Sellmeyer DE, Todd K, Sebastian A: Diet, evolution and aging–the pathophysiologic effects of the post-agricultural inversion of the potassium-to-sodium and base-to-chloride ratios in the human diet. Eur J Nutr. 2001;40(5):200–213. doi: 10.1007/s394-001-8347-4. [PubMed] [CrossRef] [Google Scholar]
27. Frassetto L, Sebastian A. Age and systemic acid-base equilibrium: analysis of published data. J Gerontol A Biol Sci Med Sci. 1996;51(1):B91–B99. [PubMed] [Google Scholar]
28. Frassetto LA, Morris RC, Sebastian A. Effect of age on blood acid-base composition in adult humans: role of age-related renal functional decline. Am J Physiol. 1996;271(6 Pt 2):F1114–F1122. [PubMed] [Google Scholar]
29. Pizzorno J, Frassetto LA, Katzinger J. Diet-induced acidosis: is it real and clinically relevant? Br J Nutr. 2010;103(8):1185–1194. [PubMed] [Google Scholar]
30. Kurtz I, Maher T, Hulter HN, Schambelan M, Sebastian A. Effect of diet on plasma acid-base composition in normal humans. Kidney Int. 1983;24(5):670–680. doi: 10.1038/ki.1983.210. [PubMed] [CrossRef] [Google Scholar]
31. Sebastian A, Frassetto LA, Sellmeyer DE, Merriam RL, Morris RC. Estimation of the net acid load of the diet of ancestral preagricultural Homo sapiens and their hominid ancestors. Am J Clin Nutr. 2002;76(6):1308–1316. [PubMed] [Google Scholar]
32. Vormann J, Goedeke T. Latent acidosis: acidity as a cause for chronic diseases [Latente Azidose: Übersäuerung als Ursache chronischer Erkrankungen] Schewiz Zschr Ganszheits Medizin. 2002;2:90–96. [Google Scholar]
33. Gluck SL. Acid-base. Lancet. 1998;352(9126):474–479. doi: 10.1016/S0140-6736(98)03087-6. [PubMed] [CrossRef] [Google Scholar]
34. Kraut JA, Madias NE. Metabolic acidosis: pathophysiology, diagnosis and management. Nat Rev Nephrol. 2010;6(5):274–285. doi: 10.1038/nrneph.2010.33. [PubMed] [CrossRef] [Google Scholar]
35. Berkemeyer S. Acid-base balance and weight gain: are there crucial links via protein and organic acids in understanding obesity? Med Hypotheses. 2009;73(3):347–356. doi: 10.1016/j.mehy.2008.09.059. [PubMed] [CrossRef] [Google Scholar]
36. Hwang JJ, Curthoys NP. Effect of acute alterations in acid-base balance on rat renal glutaminase and phosphoenolpyruvate carboxykinase gene expression. J Biol Chem. 1991;266(15):9392–9396. [PubMed] [Google Scholar]
37. Karim Z, Attmane-Elakeb A, Bichara M. Renal handling of NH4+ in relation to the control of acid-base balance by the kidney. J Nephrol. 2002;15(Suppl 5):S128–S134. [PubMed] [Google Scholar]
38. Welbourne TC. Acidosis activation of the pituitary-adrenal-renal glutaminase I axis. Endocrinology. 1976;99(4):1071–1079. doi: 10.1210/endo-99-4-1071. [PubMed] [CrossRef] [Google Scholar]
39. Espino L, Suarez ML, Santamarina G, Goicoa A, Fidalgo LE. Effects of dietary cation-anion difference on blood cortisol and ACTH levels in reproducing ewes. J Vet Med A Physiol Pathol Clin Med. 2005;52(1):8–12. doi: 10.1111/j.1439-0442.2004.00677.x. [PubMed] [CrossRef] [Google Scholar]
40. Gibson EL, Checkley S, Papadopoulos A, Poon L, Daley S, Wardle J. Increased salivary cortisol reliably induced by a protein-rich midday meal. Psychosom Med. 1999;61(2):214–224. [PubMed] [Google Scholar]
41. Slag MF, Ahmad M, Gannon MC, Nuttall FQ. Meal stimulation of cortisol secretion: a protein induced effect. Metabolism. 1981;30(11):1104–1108. doi: 10.1016/0026-0495(81)90055-X. [PubMed] [CrossRef] [Google Scholar]
42. Maurer M, Riesen W, Muser J, Hulter HN, Krapf R. Neutralization of Western diet inhibits bone resorption independently of K intake and reduces cortisol secretion in humans. Am J Physiol Renal Physiol. 2003;284(1):F32–F40. [PubMed] [Google Scholar]
43. Lemmens SG, Born JM, Martens EA, Martens MJ, Westerterp-Plantenga MS. Influence of consumption of a high-protein vs. high-carbohydrate meal on the physiological cortisol and psychological mood response in men and women. PLoS One. 2011;6(2):e16826. doi: 10.1371/journal.pone.0016826. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
44. Martens MJ, Rutters F, Lemmens SG, Born JM, Westerterp-Plantenga MS. Effects of single macronutrients on serum cortisol concentrations in normal weight men. Physiol Behav. 2010;101(5):563–567. doi: 10.1016/j.physbeh.2010.09.007. [PubMed] [CrossRef] [Google Scholar]
45. Vicennati V, Ceroni L, Gagliardi L, Gambineri A, Pasquali R. Comment: response of the hypothalamic-pituitary-adrenocortical axis to high-protein/fat and high-carbohydrate meals in women with different obesity phenotypes. J Clin Endocrinol Metab. 2002;87(8):3984–3988. doi: 10.1210/jc.87.8.3984. [PubMed] [CrossRef] [Google Scholar]
46. Zhao XY, Malloy PJ, Krishnan AV, Swami S, Navone NM, Peehl DM, Feldman D. Glucocorticoids can promote androgen-independent growth of prostate cancer cells through a mutated androgen receptor. Nat Med. 2000;6(6):703–706. doi: 10.1038/76287. [PubMed] [CrossRef] [Google Scholar]
47. Goya L, Maiyar AC, Ge Y, Firestone GL. Glucocorticoids induce a G1/G0 cell cycle arrest of Con8 rat mammary tumor cells that is synchronously reversed by steroid withdrawal or addition of transforming growth factor-alpha. Mol Endocrinol. 1993;7(9):1121–1132. doi: 10.1210/me.7.9.1121. [PubMed] [CrossRef] [Google Scholar]
48. Lippman M, Bolan G, Huff K. The effects of glucocorticoids and progesterone on hormone-responsive human breast cancer in long-term tissue culture. Cancer Res. 1976;36(12):4602–4609. [PubMed] [Google Scholar]
49. Wan Y, Nordeen SK. Overlapping but distinct gene regulation profiles by glucocorticoids and progestins in human breast cancer cells. Mol Endocrinol. 2002;16(6):1204–1214. doi: 10.1210/me.16.6.1204. [PubMed] [CrossRef] [Google Scholar]
50. Guyre PM, Girard MT, Morganelli PM, Manganiello PD. Glucocorticoid effects on the production and actions of immune cytokines. J Steroid Biochem. 1988;30(1–6):89–93. [PubMed] [Google Scholar]
51. Oxenkrug GF. Genetic and hormonal regulation of tryptophan kynurenine metabolism: implications for vascular cognitive impairment, major depressive disorder, and aging. Ann N Y Acad Sci. 2007;1122:35–49. doi: 10.1196/annals.1403.003. [PubMed] [CrossRef] [Google Scholar]
52. Katz JB, Muller AJ, Prendergast GC. Indoleamine 2,3-dioxygenase in T-cell tolerance and tumoral immune escape. Immunol Rev. 2008;222:206–221. doi: 10.1111/j.1600-065X.2008.00610.x. [PubMed] [CrossRef] [Google Scholar]
53. Opitz CA, Litzenburger UM, Sahm F, Ott M, Tritschler I, Trump S, Schumacher T, Jestaedt L, Schrenk D, Weller M. et al.An endogenous tumour-promoting ligand of the human aryl hydrocarbon receptor. Nature. 2011;478(7368):197–203. doi: 10.1038/nature10491. [PubMed] [CrossRef] [Google Scholar]
54. Prendergast GC, Metz R, Muller AJ. Towards a genetic definition of cancer-associated inflammation: role of the IDO pathway. Am J Pathol. 2011;176(5):2082–2087. [PMC free article] [PubMed] [Google Scholar]
55. Fallarino F, Gizzi S, Mosci P, Grohmann U, Puccetti P. Tryptophan catabolism in IDO + plasmacytoid dendritic cells. Curr Drug Metab. 2007;8(3):209–216. doi: 10.2174/138920007780362581. [PubMed] [CrossRef] [Google Scholar]
56. Apetoh L, Quintana FJ, Pot C, Joller N, Xiao S, Kumar D, Burns EJ, Sherr DH, Weiner HL, Kuchroo VK. The aryl hydrocarbon receptor interacts with c-Maf to promote the differentiation of type 1 regulatory T cells induced by IL-27. Nat Immunol. 2010;11(9):854–861. doi: 10.1038/ni.1912. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
57. Quintana FJ, Basso AS, Iglesias AH, Korn T, Farez MF, Bettelli E, Caccamo M, Oukka M, Weiner HL. Control of T(reg) and T(H)17 cell differentiation by the aryl hydrocarbon receptor. Nature. 2008;453(7191):65–71. doi: 10.1038/nature06880. [PubMed] [CrossRef] [Google Scholar]
58. Quintana FJ, Murugaiyan G, Farez MF, Mitsdoerffer M, Tukpah AM, Burns EJ, Weiner HL. An endogenous aryl hydrocarbon receptor ligand acts on dendritic cells and T cells to suppress experimental autoimmune encephalomyelitis. Proc Natl Acad Sci U S A. 2010;107(48):20768–20773. doi: 10.1073/pnas.1009201107. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
59. Miller LK, Kral JG, Strain GW, Zumoff B. Differential binding of dexamethasone to ammonium sulfate precipitates of human adipose tissue cytosols. Steroids. 1987;49(6):507–522. doi: 10.1016/0039-128X(87)90091-2. [PubMed] [CrossRef] [Google Scholar]
60. Rebuffe-Scrive M, Bronnegard M, Nilsson A, Eldh J, Gustafsson JA, Bjorntorp P. Steroid hormone receptors in human adipose tissues. J Clin Endocrinol Metab. 1990;71(5):1215–1219. doi: 10.1210/jcem-71-5-1215. [PubMed] [CrossRef] [Google Scholar]
61. Bujalska IJ, Kumar S, Stewart PM. Does central obesity reflect “Cushing’s disease of the omentum”? Lancet. 1997;349(9060):1210–1213. doi: 10.1016/S0140-6736(96)11222-8. [PubMed] [CrossRef] [Google Scholar]
62. Buren J, Liu HX, Jensen J, Eriksson JW. Dexamethasone impairs insulin signalling and glucose transport by depletion of insulin receptor substrate-1, phosphatidylinositol 3-kinase and protein kinase B in primary cultured rat adipocytes. Eur J Endocrinol. 2002;146(3):419–429. doi: 10.1530/eje.0.1460419. [PubMed] [CrossRef] [Google Scholar]
63. Carter-Su C, Okamoto K. Effect of glucocorticoids on hexose transport in rat adipocytes. Evidence for decreased transporters in the plasma membrane. J Biol Chem. 1985;260(20):11091–11098. [PubMed] [Google Scholar]
64. Fried SK, Russell CD, Grauso NL, Brolin RE. Lipoprotein lipase regulation by insulin and glucocorticoid in subcutaneous and omental adipose tissues of obese women and men. J Clin Invest. 1993;92(5):2191–2198. doi: 10.1172/JCI116821. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
65. Livingston JN, Lockwood DH. Effect of glucocorticoids on the glucose transport system of isolated fat cells. J Biol Chem. 1975;250(21):8353–8360. [PubMed] [Google Scholar]
66. Sakoda H, Ogihara T, Anai M, Funaki M, Inukai K, Katagiri H, Fukushima Y, Onishi Y, Ono H, Fujishiro M. et al.Dexamethasone-induced insulin resistance in 3T3-L1 adipocytes is due to inhibition of glucose transport rather than insulin signal transduction. Diabetes. 2000;49(10):1700–1708. doi: 10.2337/diabetes.49.10.1700. [PubMed] [CrossRef] [Google Scholar]
67. Turnbow MA, Smith LK, Garner CW. The oxazolidinedione CP-92,768-2 partially protects insulin receptor substrate-1 from dexamethasone down-regulation in 3T3-L1 adipocytes. Endocrinology. 1995;136(4):1450–1458. doi: 10.1210/en.136.4.1450. [PubMed] [CrossRef] [Google Scholar]
68. Frayn KN. Adipose tissue and the insulin resistance syndrome. Proc Nutr Soc. 2001;60(3):375–380. doi: 10.1079/PNS200195. [PubMed] [CrossRef] [Google Scholar]
69. Andrews RC, Walker BR. Glucocorticoids and insulin resistance: old hormones, new targets. Clin Sci (Lond) 1999;96(5):513–523. doi: 10.1042/CS19980388. [PubMed] [CrossRef] [Google Scholar]
70. Qi D, Rodrigues B. Glucocorticoids produce whole body insulin resistance with changes in cardiac metabolism. Am J Physiol Endocrinol Metab. 2007;292(3):E654–E667. [PubMed] [Google Scholar]
71. Reynolds RM, Walker BR. Human insulin resistance: the role of glucocorticoids. Diabetes Obes Metab. 2003;5(1):5–12. doi: 10.1046/j.1463-1326.2003.00221.x. [PubMed] [CrossRef] [Google Scholar]
72. Everhart J, Wright D. Diabetes mellitus as a risk factor for pancreatic cancer. A meta-analysis. JAMA. 1995;273(20):1605–1609. [PubMed] [Google Scholar]
73. Fair AM, Dai Q, Shu XO, Matthews CE, Yu H, Jin F, Gao YT, Zheng W. Energy balance, insulin resistance biomarkers, and breast cancer risk. Cancer Detect Prev. 2007;31(3):214–219. doi: 10.1016/j.cdp.2007.04.003. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
74. Giovannucci E. Insulin and colon cancer. Cancer Causes Control. 1995;6(2):164–179. doi: 10.1007/BF00052777. [PubMed] [CrossRef] [Google Scholar]
75. McKeown-Eyssen G. Epidemiology of colorectal cancer revisited: are serum triglycerides and/or plasma glucose associated with risk? Cancer Epidemiol Biomarkers Prev. 1994;3(8):687–695. [PubMed] [Google Scholar]
76. Pisani P. Hyper-insulinaemia and cancer, meta-analyses of epidemiological studies. Arch Physiol Biochem. 2008;114(1):63–70. doi: 10.1080/13813450801954451. [PubMed] [CrossRef] [Google Scholar]
77. Weiderpass E, Partanen T, Kaaks R, Vainio H, Porta M, Kauppinen T, Ojajarvi A, Boffetta P, Malats N. Occurrence, trends and environment etiology of pancreatic cancer. Scand J Work Environ Health. 1998;24(3):165–174. doi: 10.5271/sjweh.295. [PubMed] [CrossRef] [Google Scholar]
78. Kaaks R, Lukanova A, Kurzer MS. Obesity, endogenous hormones, and endometrial cancer risk: a synthetic review. Cancer Epidemiol Biomarkers Prev. 2002;11(12):1531–1543. [PubMed] [Google Scholar]
79. Wideroff L, Gridley G, Mellemkjaer L, Chow WH, Linet M, Keehn S, Borch-Johnsen K, Olsen JH. Cancer incidence in a population-based cohort of patients hospitalized with diabetes mellitus in Denmark. J Natl Cancer Inst. 1997;89(18):1360–1365. doi: 10.1093/jnci/89.18.1360. [PubMed] [CrossRef] [Google Scholar]
80. Kaaks R. Nutrition, hormones, and breast cancer: is insulin the missing link? Cancer Causes Control. 1996;7(6):605–625. doi: 10.1007/BF00051703. [PubMed] [CrossRef] [Google Scholar]
81. Stoll BA. Western nutrition and the insulin resistance syndrome: a link to breast cancer. Eur J Clin Nutr. 1999;53(2):83–87. doi: 10.1038/sj.ejcn.1600700. [PubMed] [CrossRef] [Google Scholar]
82. Gunter MJ, Hoover DR, Yu H, Wassertheil-Smoller S, Rohan TE, Manson JE, Li J, Ho GY, Xue X, Anderson GL. et al.Insulin, insulin-like growth factor-I, and risk of breast cancer in postmenopausal women. J Natl Cancer Inst. 2009;101(1):48–60. [PMC free article] [PubMed] [Google Scholar]
83. Irwin ML, Duggan C, Wang CY, Smith AW, McTiernan A, Baumgartner RN, Baumgartner KB, Bernstein L, Ballard-Barbash R. Fasting C-peptide levels and death resulting from all causes and breast cancer: the health, eating, activity, and lifestyle study. J Clin Oncol. 2011;29(1):47–53. doi: 10.1200/JCO.2010.28.4752. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
84. Kabat GC, Kim M, Caan BJ, Chlebowski RT, Gunter MJ, Ho GY, Rodriguez BL, Shikany JM, Strickler HD, Vitolins MZ. et al.Repeated measures of serum glucose and insulin in relation to postmenopausal breast cancer. Int J Cancer. 2009;125(11):2704–2710. doi: 10.1002/ijc.24609. [PubMed] [CrossRef] [Google Scholar]
85. Tran TT, Medline A, Bruce WR. Insulin promotion of colon tumors in rats. Cancer Epidemiol Biomarkers Prev. 1996;5(12):1013–1015. [PubMed] [Google Scholar]
86. Fierz Y, Novosyadlyy R, Vijayakumar A, Yakar S, LeRoith D. Insulin-sensitizing therapy attenuates type 2 diabetes-mediated mammary tumor progression. Diabetes. 2010;59(3):686–693. doi: 10.2337/db09-1291. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
87. Novosyadlyy R, Lann DE, Vijayakumar A, Rowzee A, Lazzarino DA, Fierz Y, Carboni JM, Gottardis MM, Pennisi PA, Molinolo AA. et al.Insulin-mediated acceleration of breast cancer development and progression in a nonobese model of type 2 diabetes. Cancer Res. 2010;70(2):741–751. doi: 10.1158/0008-5472.CAN-09-2141. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
88. Heuson JC, Legros N. Influence of insulin deprivation on growth of the 7,12-dimethylbenz(a)anthracene-induced mammary carcinoma in rats subjected to alloxan diabetes and food restriction. Cancer Res. 1972;32(2):226–232. [PubMed] [Google Scholar]
89. Belfiore A, Malaguarnera R. Insulin receptor and cancer. Endocr Relat Cancer. 2011;18(4):R125–R147. doi: 10.1530/ERC-11-0074. [PubMed] [CrossRef] [Google Scholar]
90. Vigneri P, Frasca F, Sciacca L, Frittitta L, Vigneri R. Obesity and cancer. Nutr Metab Cardiovasc Dis. 2006;16(1):1–7. doi: 10.1016/j.numecd.2005.10.013. [PubMed] [CrossRef] [Google Scholar]
91. Brungger M, Hulter HN, Krapf R. Effect of chronic metabolic acidosis on thyroid hormone homeostasis in humans. Am J Physiol. 1997;272(5 Pt 2):F648–F653. [PubMed] [Google Scholar]
92. Challa A, Chan W, Krieg RJ, Thabet MA, Liu F, Hintz RL, Chan JC. Effect of metabolic acidosis on the expression of insulin-like growth factor and growth hormone receptor. Kidney Int. 1993;44(6):1224–1227. doi: 10.1038/ki.1993.372. [PubMed] [CrossRef] [Google Scholar]
93. Clemmons DR, Klibanski A, Underwood LE, McArthur JW, Ridgway EC, Beitins IZ, Van Wyk JJ. Reduction of plasma immunoreactive somatomedin C during fasting in humans. J Clin Endocrinol Metab. 1981;53(6):1247–1250. doi: 10.1210/jcem-53-6-1247. [PubMed] [CrossRef] [Google Scholar]
94. Isley WL, Underwood LE, Clemmons DR. Dietary components that regulate serum somatomedin-C concentrations in humans. J Clin Invest. 1983;71(2):175–182. doi: 10.1172/JCI110757. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
95. Isley WL, Underwood LE, Clemmons DR. Changes in plasma somatomedin-C in response to ingestion of diets with variable protein and energy content. JPEN J Parenter Enteral Nutr. 1984;8(4):407–411. doi: 10.1177/0148607184008004407. [PubMed] [CrossRef] [Google Scholar]
96. Caldas A, Fontoura M. Effects of chronic metabolic acidosis (CMA) in 24-hour growth hormone secretion. J Am Soc Nephrol. 1993;4:828–828. [Google Scholar]
97. Cadogan J, Eastell R, Jones N, Barker ME. Milk intake and bone mineral acquisition in adolescent girls: randomised, controlled intervention trial. BMJ. 1997;315(7118):1255–1260. doi: 10.1136/bmj.315.7118.1255. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
98. Fontana L, Klein S, Holloszy JO. Long-term low-protein, low-calorie diet and endurance exercise modulate metabolic factors associated with cancer risk. Am J Clin Nutr. 2006;84(6):1456–1462. [PubMed] [Google Scholar]
99. Heaney RP, McCarron DA, Dawson-Hughes B, Oparil S, Berga SL, Stern JS, Barr SI, Rosen CJ. Dietary changes favorably affect bone remodeling in older adults. J Am Diet Assoc. 1999;99(10):1228–1233. doi: 10.1016/S0002-8223(99)00302-8. [PubMed] [CrossRef] [Google Scholar]
100. Schurch MA, Rizzoli R, Slosman D, Vadas L, Vergnaud P, Bonjour JP. Protein supplements increase serum insulin-like growth factor-I levels and attenuate proximal femur bone loss in patients with recent hip fracture. A randomized, double-blind, placebo-controlled trial. Ann Intern Med. 1998;128(10):801–809. [PubMed] [Google Scholar]
101. Giovannucci E, Pollak M, Liu Y, Platz EA, Majeed N, Rimm EB, Willett WC. Nutritional predictors of insulin-like growth factor I and their relationships to cancer in men. Cancer Epidemiol Biomarkers Prev. 2003;12(2):84–89. [PubMed] [Google Scholar]
102. Cohen P, Peehl DM, Rosenfeld RG. The IGF axis in the prostate. Horm Metab Res. 1994;26(2):81–84. doi: 10.1055/s-2007-1000777. [PubMed] [CrossRef] [Google Scholar]
103. LeRoith D, Baserga R, Helman L, Roberts CT. Insulin-like growth factors and cancer. Ann Intern Med. 1995;122(1):54–59. [PubMed] [Google Scholar]
104. Pollak MN. Endocrine effects of IGF-I on normal and transformed breast epithelial cells: potential relevance to strategies for breast cancer treatment and prevention. Breast Cancer Res Treat. 1998;47(3):209–217. doi: 10.1023/A:1005950916707. [PubMed] [CrossRef] [Google Scholar]
105. Chan JM, Stampfer MJ, Giovannucci E, Gann PH, Ma J, Wilkinson P, Hennekens CH, Pollak M. Plasma insulin-like growth factor-I and prostate cancer risk: a prospective study. Science. 1998;279(5350):563–566. doi: 10.1126/science.279.5350.563. [PubMed] [CrossRef] [Google Scholar]
106. Mantzoros CS, Tzonou A, Signorello LB, Stampfer M, Trichopoulos D, Adami HO. Insulin-like growth factor 1 in relation to prostate cancer and benign prostatic hyperplasia. Br J Cancer. 1997;76(9):1115–1118. doi: 10.1038/bjc.1997.520. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
107. Kaaks R, Toniolo P, Akhmedkhanov A, Lukanova A, Biessy C, Dechaud H, Rinaldi S, Zeleniuch-Jacquotte A, Shore RE, Riboli E. Serum C-peptide, insulin-like growth factor (IGF)-I, IGF-binding proteins, and colorectal cancer risk in women. J Natl Cancer Inst. 2000;92(19):1592–1600. doi: 10.1093/jnci/92.19.1592. [PubMed] [CrossRef] [Google Scholar]
108. Ma J, Giovannucci E, Pollak M, Chan JM, Gaziano JM, Willett W, Stampfer MJ. Milk intake, circulating levels of insulin-like growth factor-I, and risk of colorectal cancer in men. J Natl Cancer Inst. 2001;93(17):1330–1336. doi: 10.1093/jnci/93.17.1330. [PubMed] [CrossRef] [Google Scholar]
109. Ma J, Pollak MN, Giovannucci E, Chan JM, Tao Y, Hennekens CH, Stampfer MJ. Prospective study of colorectal cancer risk in men and plasma levels of insulin-like growth factor (IGF)-I and IGF-binding protein-3. J Natl Cancer Inst. 1999;91(7):620–625. doi: 10.1093/jnci/91.7.620. [PubMed] [CrossRef] [Google Scholar]
110. Hankinson SE, Willett WC, Colditz GA, Hunter DJ, Michaud DS, Deroo B, Rosner B, Speizer FE, Pollak M. Circulating concentrations of insulin-like growth factor-I and risk of breast cancer. Lancet. 1998;351(9113):1393–1396. doi: 10.1016/S0140-6736(97)10384-1. [PubMed] [CrossRef] [Google Scholar]
111. Zhang Y, Proenca R, Maffei M, Barone M, Leopold L, Friedman JM. Positional cloning of the mouse obese gene and its human homologue. Nature. 1994;372(6505):425–432. doi: 10.1038/372425a0. [PubMed] [CrossRef] [Google Scholar]
112. Disthabanchong S, Niticharoenpong K, Radinahamed P, Stitchantrakul W, Ongphiphadhanakul B, Hongeng S. Metabolic acidosis lowers circulating adiponectin through inhibition of adiponectin gene transcription. Nephrol Dial Transplant. 2010;26(2):592–598. [PubMed] [Google Scholar]
113. Teta D, Bevington A, Brown J, Pawluczyk I, Harris K, Walls J. Acidosis downregulates leptin production from cultured adipocytes through a glucose transport-dependent post-transcriptional mechanism. J Am Soc Nephrol. 2003;14(9):2248–2254. doi: 10.1097/01.ASN.0000083903.18724.93. [PubMed] [CrossRef] [Google Scholar]
114. Teta D, Bevington A, Brown J, Throssell D, Harris KP, Walls J. Effects of acidosis on leptin secretion from 3T3-L1 adipocytes and on serum leptin in the uraemic rat. Clin Sci (Lond) 1999;97(3):363–368. doi: 10.1042/CS19990137. [PubMed] [CrossRef] [Google Scholar]
115. Zheng F, Qiu X, Yin S, Li Y. Changes in serum leptin levels in chronic renal failure patients with metabolic acidosis. J Ren Nutr. 2001;11(4):207–211. doi: 10.1016/S1051-2276(01)70039-8. [PubMed] [CrossRef] [Google Scholar]
116. Winnicki M, Somers VK, Accurso V, Phillips BG, Puato M, Palatini P, Pauletto P. Fish-rich diet, leptin, and body mass. Circulation. 2002;106(3):289–291. doi: 10.1161/01.CIR.0000025241.01418.4D. [PubMed] [CrossRef] [Google Scholar]
117. Fung TT, Rimm EB, Spiegelman D, Rifai N, Tofler GH, Willett WC, Hu FB. Association between dietary patterns and plasma biomarkers of obesity and cardiovascular disease risk. Am J Clin Nutr. 2001;73(1):61–67. [PubMed] [Google Scholar]
118. Chu NF, Stampfer MJ, Spiegelman D, Rifai N, Hotamisligil GS, Rimm EB. Dietary and lifestyle factors in relation to plasma leptin concentrations among normal weight and overweight men. Int J Obes Relat Metab Disord. 2001;25(1):106–114. doi: 10.1038/sj.ijo.0801468. [PubMed] [CrossRef] [Google Scholar]
119. Ganji V, Kafai MR, McCarthy E. Serum leptin concentrations are not related to dietary patterns but are related to sex, age, body mass index, serum triacylglycerol, serum insulin, and plasma glucose in the US population. Nutr Metab (Lond) 2009;6:3. doi: 10.1186/1743-7075-6-3. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
120. Slieker LJ, Sloop KW, Surface PL, Kriauciunas A, LaQuier F, Manetta J, Bue-Valleskey J, Stephens TW. Regulation of expression of ob mRNA and protein by glucocorticoids and cAMP. J Biol Chem. 1996;271(10):5301–5304. doi: 10.1074/jbc.271.10.5301. [PubMed] [CrossRef] [Google Scholar]
121. Girard J. Is leptin the link between obesity and insulin resistance? Diabetes Metab. 1997;23(Suppl 3):16–24. [PubMed] [Google Scholar]
122. Kahn BB, Flier JS. Obesity and insulin resistance. J Clin Invest. 2000;106(4):473–481. doi: 10.1172/JCI10842. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
123. Heiman ML, Ahima RS, Craft LS, Schoner B, Stephens TW, Flier JS. Leptin inhibition of the hypothalamic-pituitary-adrenal axis in response to stress. Endocrinology. 1997;138(9):3859–3863. doi: 10.1210/en.138.9.3859. [PubMed] [CrossRef] [Google Scholar]
124. Korbonits M, Trainer PJ, Little JA, Edwards R, Kopelman PG, Besser GM, Svec F, Grossman AB. Leptin levels do not change acutely with food administration in normal or obese subjects, but are negatively correlated with pituitary-adrenal activity. Clin Endocrinol (Oxf) 1997;46(6):751–757. doi: 10.1046/j.1365-2265.1997.1820979.x. [PubMed] [CrossRef] [Google Scholar]
125. Remer T, Dimitriou T, Maser-Gluth C. Renal net acid excretion and plasma leptin are associated with potentially bioactive free glucocorticoids in healthy lean women. J Nutr. 2008;138(2):426S–430S. [PubMed] [Google Scholar]
126. Stephens TW, Basinski M, Bristow PK, Bue-Valleskey JM, Burgett SG, Craft L, Hale J, Hoffmann J, Hsiung HM, Kriauciunas A. et al.The role of neuropeptide Y in the antiobesity action of the obese gene product. Nature. 1995;377(6549):530–532. doi: 10.1038/377530a0. [PubMed] [CrossRef] [Google Scholar]
127. Enriori PJ, Evans AE, Sinnayah P, Cowley MA. Leptin resistance and obesity. Obesity (Silver Spring) 2006;14(Suppl 5):254S–258S. [PubMed] [Google Scholar]
128. Considine RV, Sinha MK, Heiman ML, Kriauciunas A, Stephens TW, Nyce MR, Ohannesian JP, Marco CC, McKee LJ, Bauer TL. et al.Serum immunoreactive-leptin concentrations in normal-weight and obese humans. N Engl J Med. 1996;334(5):292–295. doi: 10.1056/NEJM199602013340503. [PubMed] [CrossRef] [Google Scholar]
129. Silha JV, Krsek M, Skrha JV, Sucharda P, Nyomba BL, Murphy LJ. Plasma resistin, adiponectin and leptin levels in lean and obese subjects: correlations with insulin resistance. Eur J Endocrinol. 2003;149(4):331–335. doi: 10.1530/eje.0.1490331. [PubMed] [CrossRef] [Google Scholar]
130. Garofalo C, Surmacz E. Leptin and cancer. J Cell Physiol. 2006;207(1):12–22. doi: 10.1002/jcp.20472. [PubMed] [CrossRef] [Google Scholar]
131. Hursting SD, Perkins SN, Phang JM, Barrett JC. Diet and cancer prevention studies in p53-deficient mice. J Nutr. 2001;131(11 Suppl):3092S–3094S. [PubMed] [Google Scholar]
132. Rose DP, Komninou D, Stephenson GD. Obesity, adipocytokines, and insulin resistance in breast cancer. Obes Rev. 2004;5(3):153–165. doi: 10.1111/j.1467-789X.2004.00142.x. [PubMed] [CrossRef] [Google Scholar]
133. Somasundar P, Frankenberry KA, Skinner H, Vedula G, McFadden DW, Riggs D, Jackson B, Vangilder R, Hileman SM, Vona-Davis LC. Prostate cancer cell proliferation is influenced by leptin. J Surg Res. 2004;118(1):71–82. doi: 10.1016/j.jss.2004.01.017. [PubMed] [CrossRef] [Google Scholar]
134. Somasundar P, McFadden DW, Hileman SM, Vona-Davis L. Leptin is a growth factor in cancer. J Surg Res. 2004;116(2):337–349. doi: 10.1016/j.jss.2003.09.004. [PubMed] [CrossRef] [Google Scholar]
135. Dieudonne MN, Machinal-Quelin F, Serazin-Leroy V, Leneveu MC, Pecquery R, Giudicelli Y. Leptin mediates a proliferative response in human MCF7 breast cancer cells. Biochem Biophys Res Commun. 2002;293(1):622–628. doi: 10.1016/S0006-291X(02)00205-X. [PubMed] [CrossRef] [Google Scholar]
136. Hardwick JC, Van Den Brink GR, Offerhaus GJ, Van Deventer SJ, Peppelenbosch MP. Leptin is a growth factor for colonic epithelial cells. Gastroenterology. 2001;121(1):79–90. doi: 10.1053/gast.2001.25490. [PubMed] [CrossRef] [Google Scholar]
137. Hu X, Juneja SC, Maihle NJ, Cleary MP. Leptin–a growth factor in normal and malignant breast cells and for normal mammary gland development. J Natl Cancer Inst. 2002;94(22):1704–1711. doi: 10.1093/jnci/94.22.1704. [PubMed] [CrossRef] [Google Scholar]
138. Laud K, Gourdou I, Pessemesse L, Peyrat JP, Djiane J. Identification of leptin receptors in human breast cancer: functional activity in the T47-D breast cancer cell line. Mol Cell Endocrinol. 2002;188(1–2):219–226. [PubMed] [Google Scholar]
139. Wang Y, Kuropatwinski KK, White DW, Hawley TS, Hawley RG, Tartaglia LA, Baumann H. Leptin receptor action in hepatic cells. J Biol Chem. 1997;272(26):16216–16223. doi: 10.1074/jbc.272.26.16216. [PubMed] [CrossRef] [Google Scholar]
140. Okumura M, Yamamoto M, Sakuma H, Kojima T, Maruyama T, Jamali M, Cooper DR, Yasuda K. Leptin and high glucose stimulate cell proliferation in MCF-7 human breast cancer cells: reciprocal involvement of PKC-alpha and PPAR expression. Biochim Biophys Acta. 2002;1592(2):107–116. [PubMed] [Google Scholar]
141. Takekoshi K, Ishii K, Nanmoku T, Shibuya S, Kawakami Y, Isobe K, Nakai T. Leptin stimulates catecholamine synthesis in a PKC-dependent manner in cultured porcine adrenal medullary chromaffin cells. Endocrinology. 2001;142(11):4861–4871. doi: 10.1210/en.142.11.4861. [PubMed] [CrossRef] [Google Scholar]
142. Catalano S, Marsico S, Giordano C, Mauro L, Rizza P, Panno ML, Ando S. Leptin enhances, via AP-1, expression of aromatase in the MCF-7 cell line. J Biol Chem. 2003;278(31):28668–28676. doi: 10.1074/jbc.M301695200. [PubMed] [CrossRef] [Google Scholar]
143. Catalano S, Mauro L, Marsico S, Giordano C, Rizza P, Rago V, Montanaro D, Maggiolini M, Panno ML, Ando S. Leptin induces, via ERK1/ERK2 signal, functional activation of estrogen receptor alpha in MCF-7 cells. J Biol Chem. 2004;279(19):19908–19915. doi: 10.1074/jbc.M313191200. [PubMed] [CrossRef] [Google Scholar]
144. Bouloumie A, Drexler HC, Lafontan M, Busse R. Leptin, the product of Ob gene, promotes angiogenesis. Circ Res. 1998;83(10):1059–1066. doi: 10.1161/01.RES.83.10.1059. [PubMed] [CrossRef] [Google Scholar]
145. Park HY, Kwon HM, Lim HJ, Hong BK, Lee JY, Park BE, Jang Y, Cho SY, Kim HS. Potential role of leptin in angiogenesis: leptin induces endothelial cell proliferation and expression of matrix metalloproteinases in vivo and in vitro. Exp Mol Med. 2001;33(2):95–102. doi: 10.1038/emm.2001.17. [PubMed] [CrossRef] [Google Scholar]
146. Sierra-Honigmann MR, Nath AK, Murakami C, Garcia-Cardena G, Papapetropoulos A, Sessa WC, Madge LA, Schechner JS, Schwabb MB, Polverini PJ. et al.Biological action of leptin as an angiogenic factor. Science. 1998;281(5383):1683–1686. [PubMed] [Google Scholar]
147. Artwohl M, Roden M, Holzenbein T, Freudenthaler A, Waldhausl W, Baumgartner-Parzer SM. Modulation by leptin of proliferation and apoptosis in vascular endothelial cells. Int J Obes Relat Metab Disord. 2002;26(4):577–580. doi: 10.1038/sj.ijo.0801947. [PubMed] [CrossRef] [Google Scholar]
148. Kume K, Satomura K, Nishisho S, Kitaoka E, Yamanouchi K, Tobiume S, Nagayama M. Potential role of leptin in endochondral ossification. J Histochem Cytochem. 2002;50(2):159–169. doi: 10.1177/002215540205000204. [PubMed] [CrossRef] [Google Scholar]
149. Diez JJ, Iglesias P. The role of the novel adipocyte-derived hormone adiponectin in human disease. Eur J Endocrinol. 2003;148(3):293–300. doi: 10.1530/eje.0.1480293. [PubMed] [CrossRef] [Google Scholar]
150. Reis CE, Bressan J, Alfenas RC. Effect of the diet components on adiponectin levels. Nutr Hosp. 2010;25(6):881–888. [PubMed] [Google Scholar]
151. Koerner A, Kratzsch J, Kiess W. Adipocytokines: leptin–the classical, resistin–the controversical, adiponectin–the promising, and more to come. Best Pract Res Clin Endocrinol Metab. 2005;19(4):525–546. doi: 10.1016/j.beem.2005.07.008. [PubMed] [CrossRef] [Google Scholar]
152. Ishikawa M, Kitayama J, Kazama S, Hiramatsu T, Hatano K, Nagawa H. Plasma adiponectin and gastric cancer. Clin Cancer Res. 2005;11(2 Pt 1):466–472. [PubMed] [Google Scholar]
153. Miyoshi Y, Funahashi T, Kihara S, Taguchi T, Tamaki Y, Matsuzawa Y, Noguchi S. Association of serum adiponectin levels with breast cancer risk. Clin Cancer Res. 2003;9(15):5699–5704. [PubMed] [Google Scholar]
154. Wang Y, Lam KS, Xu JY, Lu G, Xu LY, Cooper GJ, Xu A. Adiponectin inhibits cell proliferation by interacting with several growth factors in an oligomerization-dependent manner. J Biol Chem. 2005;280(18):18341–18347. [PubMed] [Google Scholar]
155. Brakenhielm E, Veitonmaki N, Cao R, Kihara S, Matsuzawa Y, Zhivotovsky B, Funahashi T, Cao Y. Adiponectin-induced antiangiogenesis and antitumor activity involve caspase-mediated endothelial cell apoptosis. Proc Natl Acad Sci U S A. 2004;101(8):2476–2481. doi: 10.1073/pnas.0308671100. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
156. Yamauchi T, Kamon J, Ito Y, Tsuchida A, Yokomizo T, Kita S, Sugiyama T, Miyagishi M, Hara K, Tsunoda M. et al.Cloning of adiponectin receptors that mediate antidiabetic metabolic effects. Nature. 2003;423(6941):762–769. doi: 10.1038/nature01705. [PubMed] [CrossRef] [Google Scholar]
157. Gil-Campos M, Canete RR, Gil A. Adiponectin, the missing link in insulin resistance and obesity. Clin Nutr. 2004;23(5):963–974. doi: 10.1016/j.clnu.2004.04.010. [PubMed] [CrossRef] [Google Scholar]
158. Berkemeyer S. The straight line hypothesis elaborated: case reference obesity, an argument for acidosis, oxidative stress, and disease conglomeration? Med Hypotheses. 2010;75(1):59–64. doi: 10.1016/j.mehy.2009.12.034. [PubMed] [CrossRef] [Google Scholar]
159. Waris G, Ahsan H. Reactive oxygen species: role in the development of cancer and various chronic conditions. J Carcinog. 2006;5:14. doi: 10.1186/1477-3163-5-14. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
160. Malins DC, Haimanot R. Major alterations in the nucleotide structure of DNA in cancer of the female breast. Cancer Res. 1991;51(19):5430–5432. [PubMed] [Google Scholar]
161. Malins DC, Polissar NL, Gunselman SJ. Progression of human breast cancers to the metastatic state is linked to hydroxyl radical-induced DNA damage. Proc Natl Acad Sci U S A. 1996;93(6):2557–2563. doi: 10.1073/pnas.93.6.2557. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
162. Ichiba M, Maeta Y, Mukoyama T, Saeki T, Yasui S, Kanbe T, Okano J, Tanabe Y, Hirooka Y, Yamada S. et al.Expression of 8-hydroxy-2′-deoxyguanosine in chronic liver disease and hepatocellular carcinoma. Liver Int. 2003;23(5):338–345. doi: 10.1034/j.1478-3231.2003.00868.x. [PubMed] [CrossRef] [Google Scholar]
163. Schwarz KB, Kew M, Klein A, Abrams RA, Sitzmann J, Jones L, Sharma S, Britton RS, Di Bisceglie AM, Groopman J. Increased hepatic oxidative DNA damage in patients with hepatocellular carcinoma. Dig Dis Sci. 2001;46(10):2173–2178. doi: 10.1023/A:1011958814371. [PubMed] [CrossRef] [Google Scholar]
164. Feig DI, Reid TM, Loeb LA. Reactive oxygen species in tumorigenesis. Cancer Res. 1994;54(7 Suppl):1890s–1894s. [PubMed] [Google Scholar]
165. Retter AS, Gulley JL, Dahut WL. Novel therapeutic strategies in prostate cancer. Cancer Biol Ther. 2004;3(4):371–376. [PubMed] [Google Scholar]
166. Sikka SC. Role of oxidative stress response elements and antioxidants in prostate cancer pathobiology and chemoprevention–a mechanistic approach. Curr Med Chem. 2003;10(24):2679–2692. doi: 10.2174/0929867033456341. [PubMed] [CrossRef] [Google Scholar]
167. Vincent HK, Innes KE, Vincent KR. Oxidative stress and potential interventions to reduce oxidative stress in overweight and obesity. Diabetes Obes Metab. 2007;9(6):813–839. doi: 10.1111/j.1463-1326.2007.00692.x. [PubMed] [CrossRef] [Google Scholar]
168. Mayne ST. Antioxidant nutrients and chronic disease: use of biomarkers of exposure and oxidative stress status in epidemiologic research. J Nutr. 2003;133(Suppl 3):933S–940S. [PubMed] [Google Scholar]
169. Green J, Kleeman CR. Role of bone in regulation of systemic acid-base balance. Kidney Int. 1991;39(1):9–26. doi: 10.1038/ki.1991.2. [PubMed] [CrossRef] [Google Scholar]
170. Arnett T. Regulation of bone cell function by acid-base balance. Proc Nutr Soc. 2003;62(2):511–520. doi: 10.1079/PNS2003268. [PubMed] [CrossRef] [Google Scholar]
171. Bushinsky DA. Acid-base imbalance and the skeleton. Eur J Nutr. 2001;40(5):238–244. doi: 10.1007/s394-001-8351-5. [PubMed] [CrossRef] [Google Scholar]
172. Arnett TR. Acidosis, hypoxia and bone. Arch Biochem Biophys. 2010;503(1):103–109. doi: 10.1016/j.abb.2010.07.021. [PubMed] [CrossRef] [Google Scholar]
173. Arnett TR, Dempster DW. Effect of pH on bone resorption by rat osteoclasts in vitro. Endocrinology. 1986;119(1):119–124. doi: 10.1210/endo-119-1-119. [PubMed] [CrossRef] [Google Scholar]
174. Arnett TR, Spowage M. Modulation of the resorptive activity of rat osteoclasts by small changes in extracellular pH near the physiological range. Bone. 1996;18(3):277–279. doi: 10.1016/8756-3282(95)00486-6. [PubMed] [CrossRef] [Google Scholar]
175. Goldhaber P, Rabadjija L. H + stimulation of cell-mediated bone resorption in tissue culture. Am J Physiol. 1987;253(1 Pt 1):E90–E98. [PubMed] [Google Scholar]
176. Kraut JA, Mishler DR, Kurokawa K. Effect of colchicine and calcitonin on calcemic response to metabolic acidosis. Kidney Int. 1984;25(4):608–612. doi: 10.1038/ki.1984.64. [PubMed] [CrossRef] [Google Scholar]
177. Bushinsky DA, Krieger NS, Geisser DI, Grossman EB, Coe FL. Effects of pH on bone calcium and proton fluxes in vitro. Am J Physiol. 1983;245(2):F204–F209. [PubMed] [Google Scholar]
178. Bushinsky DA. Net calcium efflux from live bone during chronic metabolic, but not respiratory, acidosis. Am J Physiol. 1989;256(5 Pt 2):F836–F842. [PubMed] [Google Scholar]
179. Frick KK, Bushinsky DA. Metabolic acidosis stimulates RANKL RNA expression in bone through a cyclo-oxygenase-dependent mechanism. J Bone Miner Res. 2003;18(7):1317–1325. doi: 10.1359/jbmr.2003.18.7.1317. [PubMed] [CrossRef] [Google Scholar]
180. Boyle WJ, Simonet WS, Lacey DL. Osteoclast differentiation and activation. Nature. 2003;423(6937):337–342. doi: 10.1038/nature01658. [PubMed] [CrossRef] [Google Scholar]
181. Chang L, Karin M. Mammalian MAP kinase signalling cascades. Nature. 2001;410(6824):37–40. doi: 10.1038/35065000. [PubMed] [CrossRef] [Google Scholar]
182. Nakashima T, Kobayashi Y, Yamasaki S, Kawakami A, Eguchi K, Sasaki H, Sakai H. Protein expression and functional difference of membrane-bound and soluble receptor activator of NF-kappaB ligand: modulation of the expression by osteotropic factors and cytokines. Biochem Biophys Res Commun. 2000;275(3):768–775. doi: 10.1006/bbrc.2000.3379. [PubMed] [CrossRef] [Google Scholar]
183. Wada T, Penninger JM. Mitogen-activated protein kinases in apoptosis regulation. Oncogene. 2004;23(16):2838–2849. doi: 10.1038/sj.onc.1207556. [PubMed] [CrossRef] [Google Scholar]
184. Leibbrandt A, Penninger JM. RANK/RANKL: regulators of immune responses and bone physiology. Ann N Y Acad Sci. 2008;1143:123–150. doi: 10.1196/annals.1443.016. [PubMed] [CrossRef] [Google Scholar]
185. Gonzalez-Suarez E. RANKL inhibition: a promising novel strategy for breast cancer treatment. Clin Transl Oncol. 2011;13(4):222–228. doi: 10.1007/s12094-011-0646-5. [PubMed] [CrossRef] [Google Scholar]
186. Ishida N, Hayashi K, Hoshijima M, Ogawa T, Koga S, Miyatake Y, Kumegawa M, Kimura T, Takeya T. Large scale gene expression analysis of osteoclastogenesis in vitro and elucidation of NFAT2 as a key regulator. J Biol Chem. 2002;277(43):41147–41156. doi: 10.1074/jbc.M205063200. [PubMed] [CrossRef] [Google Scholar]
187. Takayanagi H, Kim S, Koga T, Nishina H, Isshiki M, Yoshida H, Saiura A, Isobe M, Yokochi T, Inoue J. et al.Induction and activation of the transcription factor NFATc1 (NFAT2) integrate RANKL signaling in terminal differentiation of osteoclasts. Dev Cell. 2002;3(6):889–901. doi: 10.1016/S1534-5807(02)00369-6. [PubMed] [CrossRef] [Google Scholar]
188. Komarova SV, Pereverzev A, Shum JW, Sims SM, Dixon SJ. Convergent signaling by acidosis and receptor activator of NF-kappaB ligand (RANKL) on the calcium/calcineurin/NFAT pathway in osteoclasts. Proc Natl Acad Sci U S A. 2005;102(7):2643–2648. doi: 10.1073/pnas.0406874102. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
189. Mancini M, Toker A. NFAT proteins: emerging roles in cancer progression. Nat Rev Cancer. 2009;9(11):810–820. doi: 10.1038/nrc2735. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
190. Buchholz M, Schatz A, Wagner M, Michl P, Linhart T, Adler G, Gress TM, Ellenrieder V. Overexpression of c-myc in pancreatic cancer caused by ectopic activation of NFATc1 and the Ca2+/calcineurin signaling pathway. EMBO J. 2006;25(15):3714–3724. doi: 10.1038/sj.emboj.7601246. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
191. Holzmann K, Kohlhammer H, Schwaenen C, Wessendorf S, Kestler HA, Schwoerer A, Rau B, Radlwimmer B, Dohner H, Lichter P. et al.Genomic DNA-chip hybridization reveals a higher incidence of genomic amplifications in pancreatic cancer than conventional comparative genomic hybridization and leads to the identification of novel candidate genes. Cancer Res. 2004;64(13):4428–4433. doi: 10.1158/0008-5472.CAN-04-0431. [PubMed] [CrossRef] [Google Scholar]
192. Koenig A, Linhart T, Schlengemann K, Reutlinger K, Wegele J, Adler G, Singh G, Hofmann L, Kunsch S, Buch T. et al.NFAT-induced histone acetylation relay switch promotes c-Myc-dependent growth in pancreatic cancer cells. Gastroenterology. 2010;138(3):1189-1199 e1181-1182. [PMC free article] [PubMed] [Google Scholar]
193. Masuo T, Okamura S, Zhang Y, Mori M. Cyclosporine A inhibits colorectal cancer proliferation probably by regulating expression levels of c-Myc, p21(WAF1/CIP1) and proliferating cell nuclear antigen. Cancer Lett. 2009;285(1):66–72. doi: 10.1016/j.canlet.2009.05.001. [PubMed] [CrossRef] [Google Scholar]
194. Singh G, Singh SK, Konig A, Reutlinger K, Nye MD, Adhikary T, Eilers M, Gress TM, Fernandez-Zapico ME, Ellenrieder V. Sequential activation of NFAT and c-Myc transcription factors mediates the TGF-beta switch from a suppressor to a promoter of cancer cell proliferation. J Biol Chem. 2010;285(35):27241–27250. doi: 10.1074/jbc.M110.100438. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
195. Schwalfenberg GK. The alkaline diet: is there evidence that an alkaline pH diet benefits health? J Environ Public Health. 2012;2012:727630. [PMC free article] [PubMed] [Google Scholar]